Case Report
Osteogenic Accelerated OrthodonticsTM for treatment of a Skeletal Class II patient with moderate crowding

Armando Montesinos F1 and Marisol Pérez Gasque B2
1Department of Orthodontics, Postgraduate Studies and Research Division, Odontology Faculty, National Autonomous University of Mexico, Mexico
2Department of Implantology, Postgraduate Studies and Research Division, Odontology Faculty, National Autonomous University of Mexico, Mexico
*Address for Correspondence: Armando Montesinos F, Department of Orthodontics, Postgraduate Studies and Research Division, Odontology Faculty, National Autonomous University of Mexico, Mexico, Email: [email protected]
Dates: Submitted: 01 August 2017; Approved: 15 September 2017; Published: 18 September 2017
How to cite this article: Armando Montesinos F, Marisol Pérez Gasque B. Osteogenic Accelerated OrthodonticsTM for treatment of a Skeletal Class II patient with moderate crowding. J Oral Health Craniofac Sci. 2017; 2: 083-089. DOI: 10.29328/journal.johcs.1001016
Copyright License: 2017 Armando Montesinos F, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Introduction: A 17 years old male patient was treated at the University orthodontic department. He had the chief complaint of unaesthetic appearance of his teeth, mostly for anterior crowding. The pretreatment records showed a Class II skeletal relation, moderate upper and lower anterior crowding, 0.5mm of overbite and 2mm of overjet.
Materials and Methods: It was suggested Osteogenic Accelerated Orthodontics (OAOTM), the treatment option was very attractive to the patient although it required a surgical procedure and a more expensive type of treatment.
Results: The overall treatment time was 6 months, facial balance was improved and the final occlusal relationships from the functional and aesthetics perspective were good.
Conclusion: OAOTM is a good alternative to reduce extractions rate as it increases the scope of tooth movement and strengthen the periodontal tissues thru bone grafting, although these claims require more scientific data to be validated.
Introduction
Orthodontic treatment in the 21st century has evolved at great speed, new technology is incorporated in diagnostic tools, and materials science and engineering have designed new materials and manufacturing processes that are applied in the orthodontic industry. Current biological concepts of tooth movement and growth and development of humans are more complex and new philosophies and treatment options are available for the patient and orthodontist. Contemporary treatment objectives are: function, facial balance, stability of the dentition and periodontal integrity. These objectives are routinely obtained thru a variety of treatment philosophies and techniques. One of the current tendencies is the surgical facilitated orthodontics for the reduction of treatment time; human beings are living a fast paced world, so they request a fast option of treatment.
Diagnosis and etiology
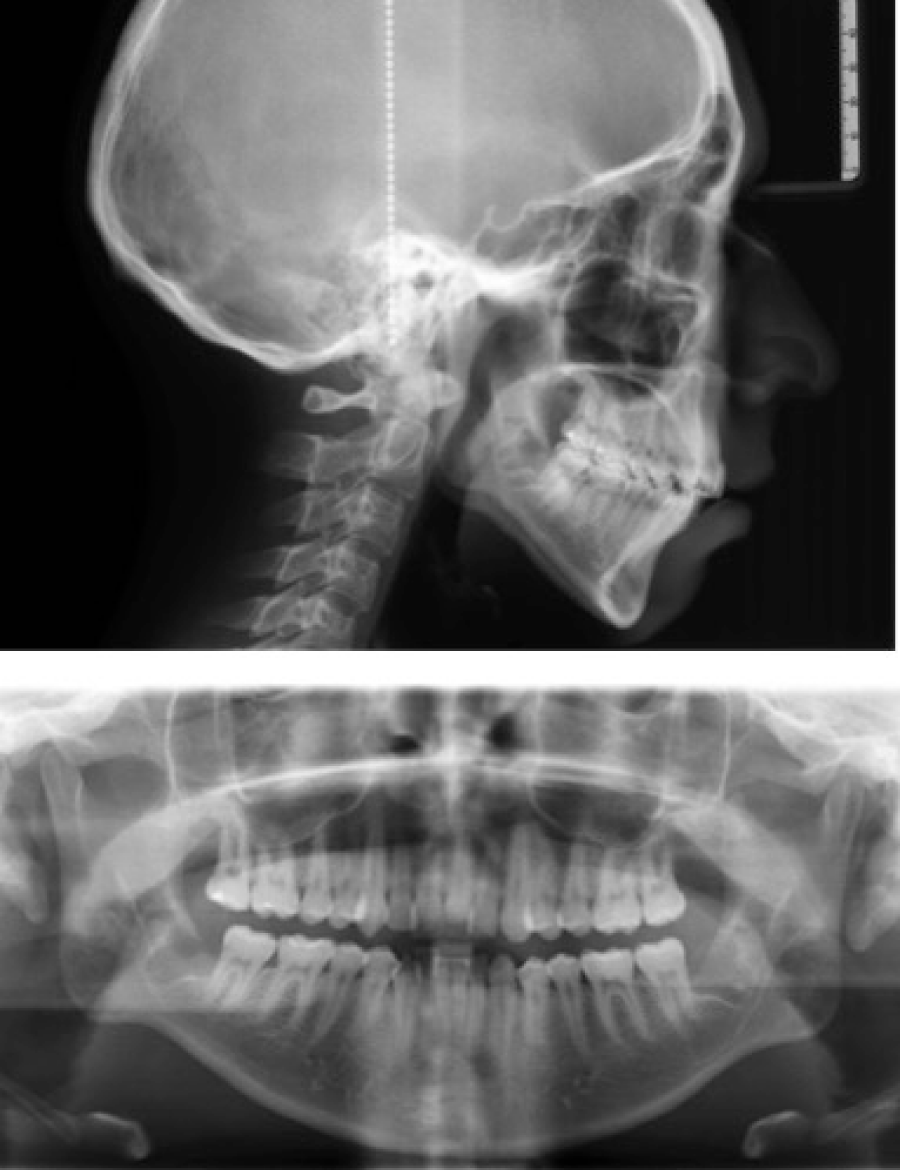
A 17 years old male patient came to the University orthodontic department with the chief complaint of crowding in the anterior region (Figure 1). He had no significant medical history. The pretreatment records showed a Class II skeletal relation and vertical pattern (Table 1 and Figure 2). The dental findings were an Angle Class I molar relationship, moderate upper and lower anterior crowding, 0.5mm of overbite and 2mm of overjet. The panoramic radiograph showed lack of dental roots parallelism (Figure 2).
| Table 1. Cephalometric measurements | |||
| Measurement | Norm | Pretreatment | Posttreament |
| SNA | 82° | 85° | 85° |
| SNB | 80° | 80° | 80° |
| ANB | 2° | 5° | 5° |
| Go Gn-SN | 40° | 40° | 40° |
| Facial Axis | 90° | 86° | 86° |
| 1-1 | 130° | 130° | 128° |
| 1-SN | 102° | 99° | 102° |
| IMPA | 90° | 91° | 95° |
| Profile | |||
| Upper lip-E line (mm) | 1 to -4mm | 0mm | 0mm |
| Lower lip-E line (mm) | 0 to 2mm | 0mm | 1mm |
Treatment objectives
The treatment objectives for this case were to [1], eliminate dental crowding [2], achieve better facial balance [3], maintain a Class I dental relationship [4] maintain the root length of the teeth.
Treatment alternatives
One of the patient´s concerns was dental extraction and the duration of conventional orthodontic treatment, so it was suggested Osteogenic Accelerated Orthodontics (OAOTM) to reduce treatment time and to enhance the scope of orthodontic treatment. The second option was conventional orthodontic treatment with four first bicuspid extractions to relieve crowding. The patient selected the OAOTM treatment option, although it required a surgical procedure and a more expensive type of treatment.
Treatment progress
One week before surgery 0.022” x 0.028” MBT (3M Unitek, Monrovia, CA) appliance was bonded but no archwires were engaged. A surgical map drawn by the orthodontist was used to communicate with the periodontist to indicate where the corticotomies were required. Full thickness flaps facially and lingually were made and alveolar selective corticotomies were performed with a Piezotome (Satelec Acteon Group, France), using the BS1Slim tip (F87525), drawing the radicular anatomy of each tooth; the bone grafting used was a mixture of 1 gram of bovine bone (NuOssTM, ACE Surgical Supply Co., Inc. Brockton, MA), 2 grams of demineralized bone matrix (Biograft), and 500 mg of metronidazole in saline solution (10cc), Vicryl 4-0 (Ethicon Endo-Surgery, Inc. Cincinnati, OH) was the suture material in both arches (Figure 4).
After surgery Niti 0.014” archwires were engaged and appointments were scheduled every two weeks from start to finish of treatment. The level and aligning phase was obtained thru Niti archwires (0.014”, 0.016”, 0.016” x 0.022” and 0.019” x 0.025”) upper and lower right lateral incisors were not tied to the arch because lack of space. A Niti open coil was inserted between lower right central and cusped upper and lower; when space was created a sectional 0.012” Niti was engaged to align upper and lower right lateral incisors (Figure 3). Coordinated upper and lower 0.019” x 0.025” SS archwires were engaged and a panoramic radiograph was taken to check root alignment and bracket repositioning, Niti 0.016” x 0.022” upper and lower archwires were engaged; the following archwires were used in the posterior appointments Niti 0.017” x 0.025”, 0.019” x 0.025” and SS 0.019” x 0.025” for finishing and detailing. Brackets were debonded and the retention protocol was upper and lower circumferential retainers 24 hours a day.
Figure 4: Surgical procedure: Full thickness flaps reflection, selective alveolar corticotomies, teeth extractions and bone grafting mixture.
Treatment results
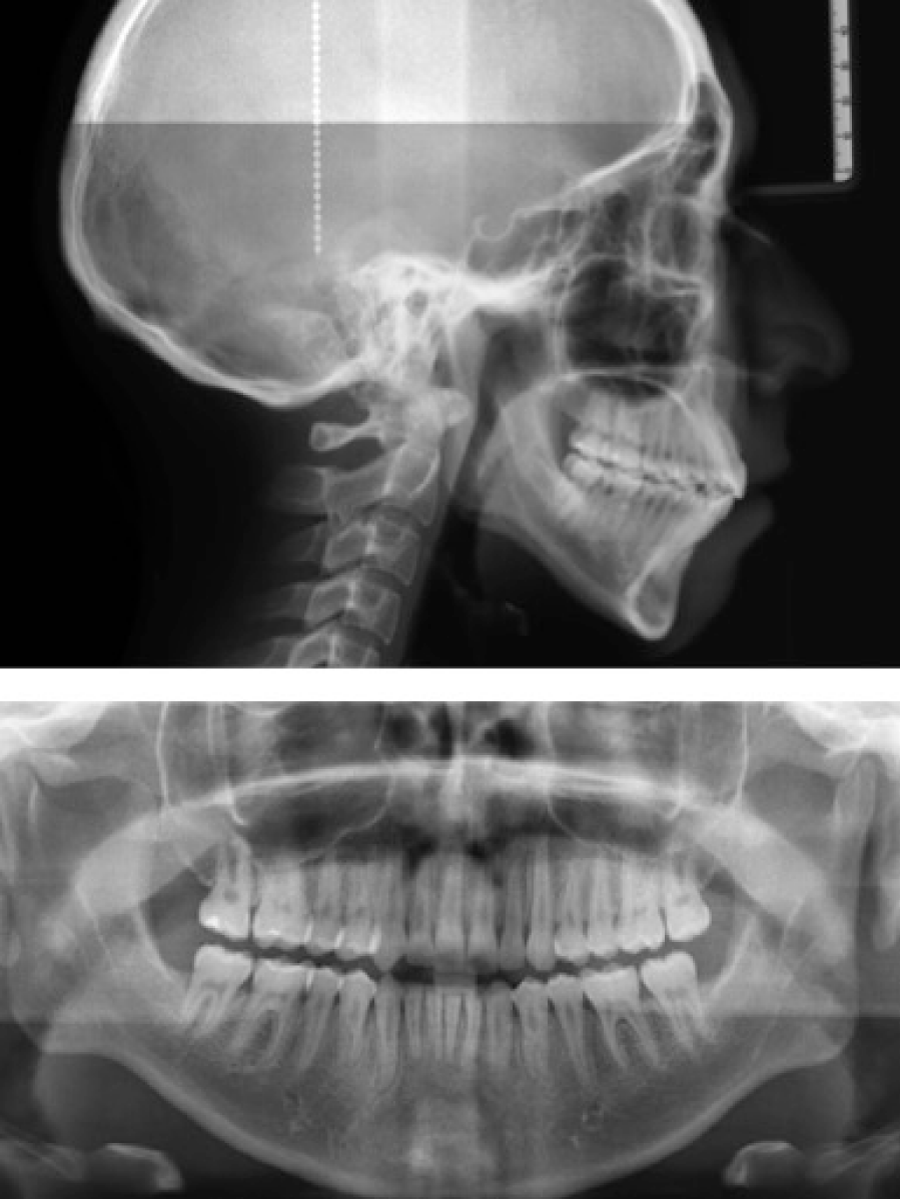
The overall treatment time was 6 months and there were no complications during and after the surgical procedure Facial balance was improved and the final occlusal relationships were good (Figure 5). Dental crowding was relieved thru mild expansion of the arches and proclination of upper and lower arches; it should be highlighted that the degree of proclination was very mild. Good parallelism of roots was also achieved (Table 1 and Figure 6).
Discussion
The world has evolved into a fast paced environment, human beings want everything fast, fast results from a health product, new workout system for faster results, fast achievements, fast service, etc. It seems that “fast” can be equal to “good”, so a faster service or faster results means a better one, premise that is not “true”. Orthodontics has been influenced by this “I want it fast…” posture as well; the main burdens about orthodontic appliances are aesthetics concerns, plaque retention, discomfort caused by orthodontic forces and irritated mucosa (cheeks and lips). Orthodontic patients experience pain and discomfort to a varying degree during the course of treatment [1], but it must be considered that the interpretation of discomfort and pain is subjective; low intensity forces and state of the art manufacture processes to fabricate brackets are applied to diminished patient discomfort. The aesthetics concerns are related to the visibility of metal braces bonded into a beautiful aesthetic structure, as it is the enamel of the teeth; clear braces are available but still are noticeable unless concealed braces are worn. Poor oral hygiene and plaque retention control can lead to white spot lesions, gingivitis and cavities and periodontal disease in more severe cases. Therefore if the orthodontic treatment length can be shortened the risks can be less and the time the aesthetics of the patient can be compromised shortened; although every clinician knows that patients adapt very well to orthodontic therapy and good hygiene habits can be established.
Accelerated tooth movement had a fast evolution; it has a variety of approaches that includes surgical techniques and no surgical modalities [2], such as micro vibration [3], light stimulation [4], pharmacological approaches [5], etc. The surgical facilitated orthodontic treatment protocol is very popular and different authors have established a particular sequence of procedures or specific steps to name, rename or patent a particular technique, for example: Wilckodontics (OAOTM) [6-10], Piezosurgery [11], Piezocision [12], Speedy orthodontics [13,14]. Propel Orthodontics (micro-osteoperforations) [15].
The surgical facilitated orthodontic treatment protocol requires a corticotomy procedure: a shallow perforation or cuts made on the alveolar bone only [16]. All different surgical approaches share the same biologic mechanism: “a regional acceleratory phenomenon (RAP)” concept developed by Frost and Jee and described in the periodontal literature by Yafee and coworkers [9,17]. This phenomenon affects bone healing pattern and turnover, so as a consequence: a temporary phase of accelerated tooth movement [9].
Micro-osteoperforations (MOPs) practitioners explain the accelerated tooth movement by another biological principle, Texeira et al., reported that performing MOPs on alveolar bone during orthodontic tooth movement can stimulate the expression of inflammatory markers, leading to increases in osteclastic activity and the rate of tooth movement [18]. MOPs significantly increase the expression of cytokines and chemokines known to recruit osteoclast precursors and stimulate osteoclast differentiation and that MOPs are an effective, comfortable and safe procedure to accelerate tooth movement during orthodontic treatment [15].
The bottom line of all the different surgical facilitated orthodontics approaches is an accelerated tooth movement; creators and developers of the different treatment protocols claim advantages and disadvantages between the techniques. The main concerns have been the invasiveness, discomfort and the risks involved during the surgical time and post-surgery. The most invasive protocols are Wilckodontics [6-10] and Piezosurgery [11], as they require full thickness flaps to make the corticotomies. Piezocision technique requires microsurgical interproximal openings made in the buccal gingivae to let the piezoelectric knife create the bone injury diminishing the invasiveness of the surgical procedure [19]. Propel Orthodontics is considered the least invasive as the MOPs are made with a handheld appliance thru the mucosa [15].
The case described can be a good example how a new or different approach of treatment can cause controversy. In a traditional approach treating the case within the dimensions of the denture [20], this patient could be considered as a typical four first bicuspid extractions case but with surgical facilitated orthodontics the scope of orthodontic tooth movement can be increased [8,21] therefore in this case dental extractions were not done. It must be emphasized that alveolar augmentation was performed to strengthen the periodontal tissue; it is the third element of OAOTM: orthodontic forces, selective alveolar corticotomies and alveolar augmentation. The anterior crowding was relieved by expansion of the arches, mild proclination of the upper and lower incisors is observed in the cephalometric measurements (Table 1) and good alveolar width is observed in posttreatment CBCT scan in the lower arch (Figure 7).
The highlight is that one of the claimed advantages of surgical facilitated orthodontics specifically OAOTM is to reduce extraction decisions as the scope of treatment is enhanced and the periodontal tissue strengthen thru bone grafting although these claims need more scientific data to be validated. The counterpoint is that orthodontist must diagnose objectively cases and plan orthodontic treatment without the influence of norms, philosophy or technique that promise to reduce extractions or miraculously change the orthodontic scene as propose by an orthodontic guru or maybe an academic who represents a new bracket design or orthodontic products. Nevertheless surgical facilitated orthodontics really can change treatment paradigms, as the scope of tooth movement is increased [8,21].
In regard of the different techniques in must be pointed out that there is a tendency to be minimally invasive and aggressive in the surgical procedures as in all medical fields, although tissue injury is needed to generate the maximum RAP. It can be considered a disadvantage of the protocols requiring flap surgery to make the corticotomies because the increased invasiveness and risks over the protocols that don´t, but certainly it is an advantage in terms of visibility and precision of the corticotomies, reducing the risk of cutting unwanted sites such as a dental root.
Conclusion
1. OAOTM is a good alternative to reduce extractions rate as it increases the scope of tooth movement and strengthen the periodontal tissues thru bone grafting, although these claims require more scientific data to be validated.
2. Conventional orthodontic cases must be treated within the dimensions of the denture, making dental extractions decisions as needed.
Acknowledgements
We thank the collaboration of Dr. Leticia Bernal orthodontic resident for being part of the team involved in the patient treatment.
References
- Sergl HG, Klages U, Zentner A. Pain and discomfort during orthodontic treatment: causative factores and effects on compliance. Am J Orthod Dentofacial Orthop. 1998; 114: 648-691. Ref.: https://goo.gl/WXpkN5
- Long H, Pyakurel U, Wang Y, Liao L, Zhou Y, et al. Interventions for accelerating orthodontic tooth movement: a systematic review. Angle Orthod. 2013; 83: 164-171. Ref.: https://goo.gl/jjhmPx
- Nishimura M, Chiba M, Ohashi T, Sato M, Shimizu Y, et al. Periodontal tissue activation by vibration: intermittent stimulation by resonance vibration accelerates experimental tooth movement in rats. Am J Orthod Dentofacial Orthop. 2008; 133: 572-583. Ref.: https://goo.gl/g4VZXF
- Kau CH, Kantarci A, Shaughnessy T, Vachiramon A, Santiwong P, et al. Photobiomodulation accelerates orthodontic alignment in the early phase of treatment. Prog Orthod. 2013; 14: 30. Ref.: https://goo.gl/953km1
- Kanzaki H, Chiba M, Arai K, Takahashi I, Haruyama N, et al. Local RANKL gene transfer to the periodontal tissue accelerates orthodontic tooth movement. Gene Ther. 2006; 13: 678-685. Ref.: https://goo.gl/gW9g1z
- Murphy KG, Wilcko MT, Wilcko WM, Ferguson DJ. Periodontal Accelerated Osteogenic Orthodontics. A Description of the Surgical Technique. J Oral Maxillofac Surg. 2009; 67: 2160-2166. Ref.: https://goo.gl/51wtLk
- Wilcko WM, Wilcko MT, Bouquot JE, Ferguson DJ. Accelerated orthodontics with alveolar reshaping. J Ortho Practice. 2000; 10: 63-70.
- Wilcko WM, Ferguson DJ, Bouquot JE, Wilko MT. Rapid orthodontic decrowding with alveolar augmentation: case report. World J Orthod. 2003; 4: 197-205. Ref.: https://goo.gl/cCo9ar
- Wilcko MT, Wilcko WM, Bissada NF. An evidence-based analysis of periodontally accelerated orthodontic and osteogenic techniques a synthesis of scientific perspective. Seminars Orthod. 2008; 14: 305-316. Ref.: https://goo.gl/U5tDcf
- Wilcko MT, Wilcko WM, Pulver JJ, Bissada NF, Bouquot JE. Accelerated osteogenic orthodontics technique: A 1-stage surgically facilitated rapid orthodontic technique with alveolar augmentation. J Oral Maxillofac Surg. 2009; 67: 2149-2159. Ref.: https://goo.gl/FMVh37
- Vercellotti T, Podesta A. Orthodontic Microsurgery: A new surgically guided technique for dental movement. Int J Periodontics Restorative Dent. 2007; 27: 325-331. Ref.: https://goo.gl/9PyojS
- Dibart S, Sebaoun JD, Surmenian J. Piezocision: a minimal invasive, periodontally accelerated orthodontic movement procedure. Compend Contin Educ Dent. 2009; 30: 342-344. Ref.: https://goo.gl/UMbHZa
- Chung K, Kim S, Lee B. Speedy surgical-orthodontic treatment with temporary anchorage devices as an alternative to orthognathic surgery. Am J Orthod Dentofacial Orthop. 2009; 135: 787-798. Ref.: https://goo.gl/5NMww8
- Chung K, Mitsugi M, Lee B, Kanno T, Lee W, et al. Speedy surgical orthodontic treatment with skeletal anchorage in adults-sagittal correction and open bite correction. J Oral Maxillofac Surg. 2009; 67: 2130-2148. Ref.: https://goo.gl/4ETjTp
- Alikhani M, Raptis M, Zoldan B, Sangsuwon C, Lee YB, et al. Effect of micro-osteoperforations on the rate of tooth movement. Am J Orthod Dentofacial Orthop. 2013; 144: 639-648. Ref.: https://goo.gl/S1Qbsq
- Hoogeveen EJ, Jansama J, Ren Y. Surgically facilitated orthodontic treatment: a systematic review. Am J Orthod Dentofacial Orthop. 2014; 145: 51-64. Ref.: https://goo.gl/4QviQF
- Yaffe A, Fine N, Binderman I. Regional accelerated phenomenon in the mandible following mucoperiosteal flap surgery. J Periodontal. 1994; 65: 79-83. Ref.: https://goo.gl/yLA7mb
- Teixeira CC, Khoo E, Tran J, Chartres I, Liu Y, et al. Cytokine expression and accelerated tooth ovement. J Dent Res. 2010; 89: 1135-1141. Ref.: https://goo.gl/QGf4iD
- Keser EI, Dibart S. Sequential piezocision a novel approach to accelerated orthodontic treatment. Am J Orthod Dentofacial Orthop. 2013; 144: 879-889. Ref.: https://goo.gl/21CrMQ
- Merrifield LL. Dimensions of the denture:back to basics. AM J Orthod Dentofacial Orthop. 1994; 106: 535-542. Ref.: https://goo.gl/2AzCrS
- Ferguson DJ, Wilcko WM, Wilcko MT. Selective alveolar decortication for rapid surgical-orthodontic resolution of skeletal malocclusion treatment, in Bell WE, Guerrero c (eds): Distraction Osteogenesis of the Facial Skeleton. Hamilton BC Decker. 2006; 199-203.