More Information
Submitted: November 24, 2022 | Approved: December 06, 2022 | Published: December 09, 2022
How to cite this article: Carrafiello A. Recovery of craniofacial proportions using the Nuvola Op System protocol. J Oral Health Craniofac Sci. 2022; 7: 022-026.
DOI: 10.29328/journal.johcs.1001041
Copyright License: © 2022 Carrafiello A. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Recovery of craniofacial proportions using the Nuvola Op System protocol
Alessandro Carrafiello*
M.D., D.M.D., Private Practice, 42122 Reggio Emilia, Italy
*Address for Correspondence: Dr. Alessandro Carrafiello, M.D., D.M.D., Private Practice, 42122 Reggio Emilia, Italy, Email: [email protected]
The stomatognathic apparatus is currently understood as a complex functional unit in its muscular, skeletal, dental, and neurological parts; in particular, it is now commonly acknowledged that the craniofacial district is connected to the type of occlusion not only functionally but also morphologically. Occlusion is the result of the adaptation of dental organs that can adapt through the periodontium and cranial bones through sutures, with the “neurological direction” of the function and tone of the perioral, lingual, and craniocervical muscles.
The perceived aesthetic aspect of harmony is unrelated to these concepts. If the required adaptations to the stomatognathic system led to morphologically asymmetrical results, which may result in a negative perception.
Face and proportions
Since antiquity, fundamental parameters capable of linking form and harmony have been recognized, starting with Polyclitus, but it is then with Leonardo da Vinci and Luca Pacioli that we arrive at mathematical proportion, whose irrational number 1.6180339887 finds multiple applications, from geometry to art and nature. This mathematical proportion constantly recurs in the human face, also whenever an unconscious and harmonious perception is sought. The functional planning of the OP System considers palatal transversality and frontal dental visual impact according to these canons; final volumetric control then confirmed a good recovery of facial symmetry [1-5].
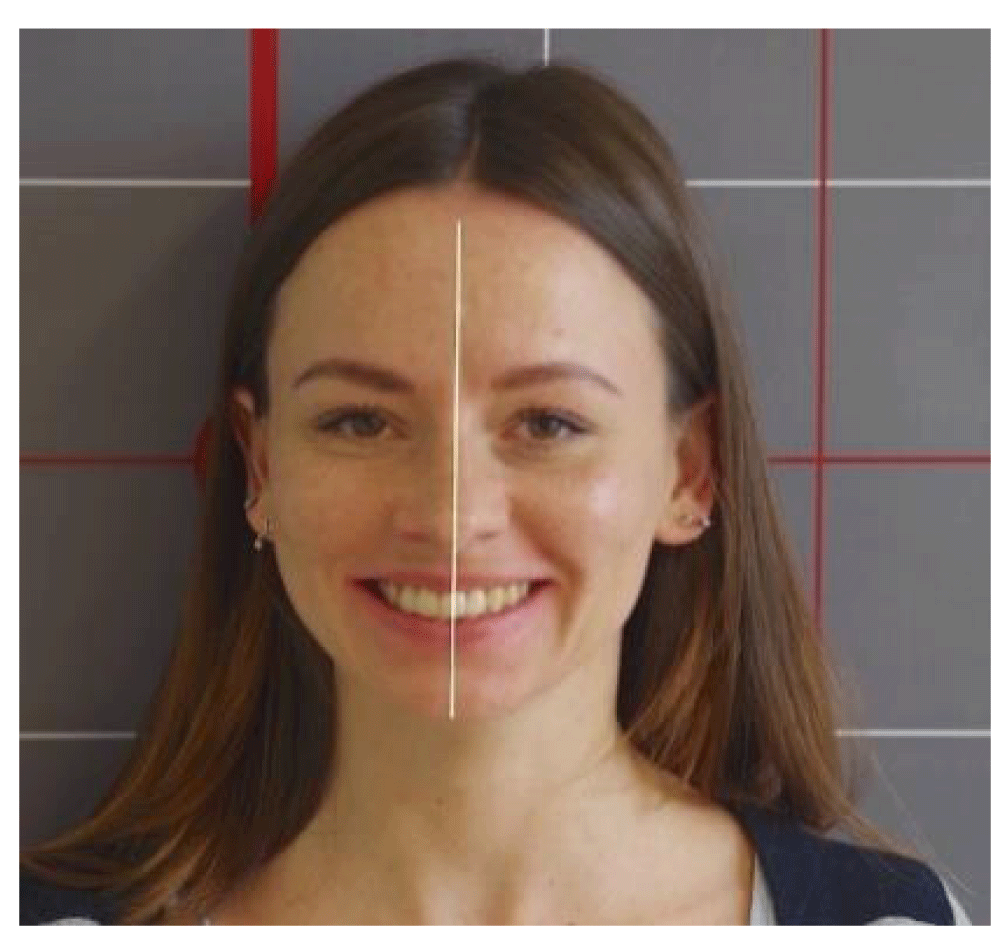
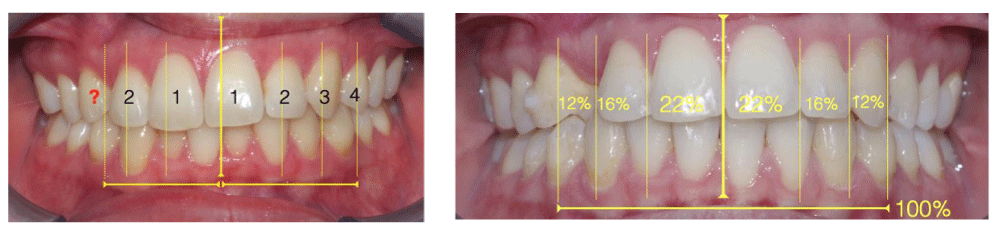
In the case reported in this article, the main goal is the recovery of transversality that is harmoniously placed in the facial framework and allows the reconstruction of a centered and natural dental aesthetic (Figures 1,2).
Figure 1: Pretreatment facial photograph.
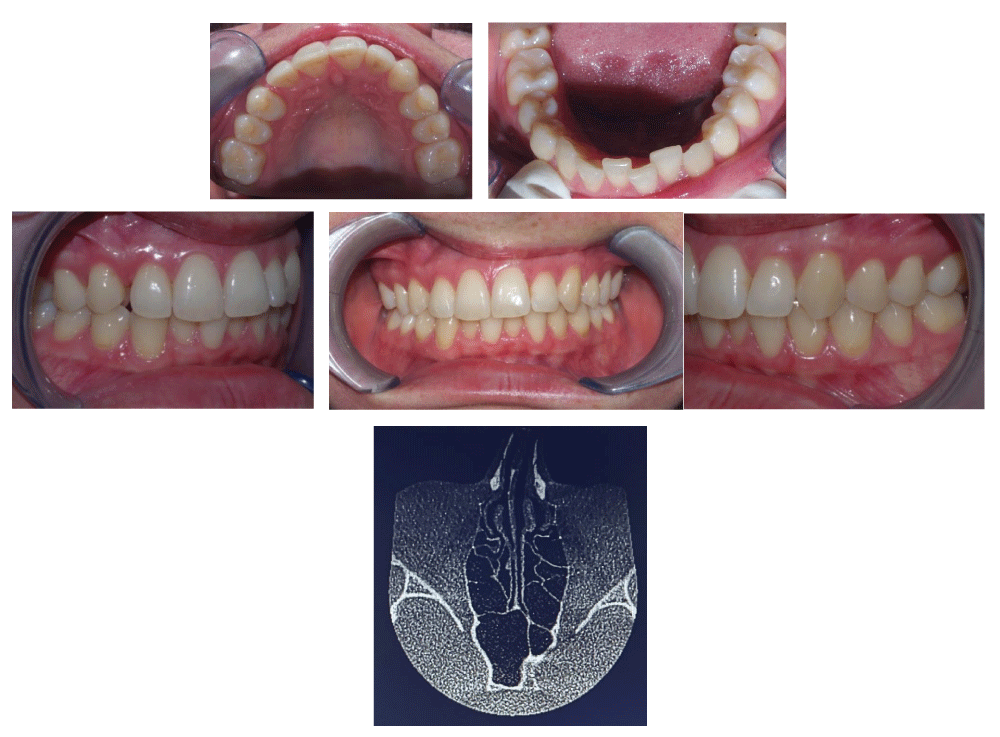
Figure 2a-f: Pretreatment intraoral photographs and CT slice showing deviated nasal cavities.
To achieve this, a female adult patient was treated with a new orthodontic protocol proposed by Nuvola® (G.E.O. S.r.l., Rome, Italy) called OP System™ has existed since 2019. The system combines specifically designed aligners with the use of a prefabricated myofunctional appliance (PFA) called Freedom™ and specifically designed aligners. PFAs are removable orthodontic devices made of an elastomeric material that integrates soft shields around the upper and lower arch. These devices aim to correct malocclusions and can be worn a few hours a day. PFAs are soft, non-personalized, and often used in conjunction with myofunctional exercises. Their historical existence dates back several decades and published clinical studies compared their effects with more traditional functional appliances.
The OP system protocol
The Op System Protocol consists of two closely related components:
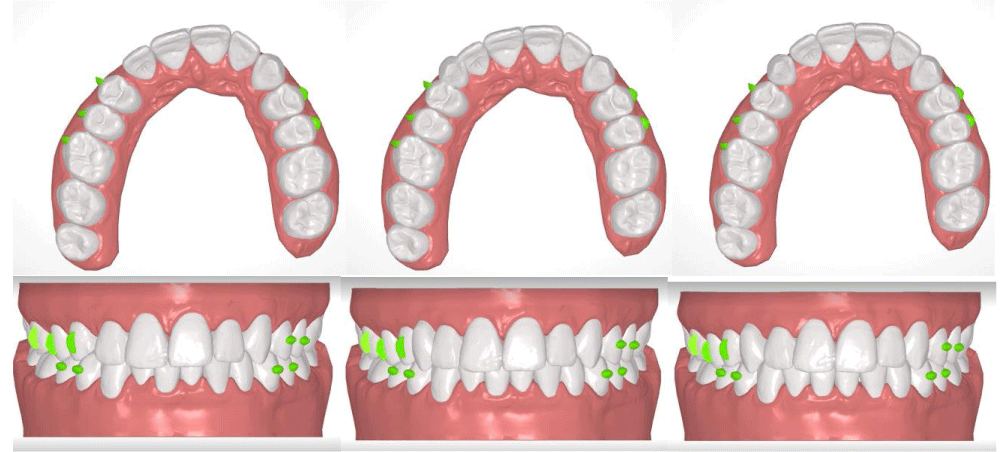
1. Aligners with a specific design called Nuvola Pro™ (Figure 3).
Figure 3(a-c): The Nuvola Pro™ aligners are specifically designed for the OP System protocol. Images 4b and 4c show in blue respectively the lingual pins and reinforced areas.
2. Elastic device Freedom™ (Figure 4).
Figure 4: The Freedom device presents alternated shields and a central tongue guide.
The aligners have palatal reinforcement areas that, when subjected to adequate pressure allow a slight deformation which corresponds to each palatal area divided by its sutures (Figure 3c). The reinforced areas of the aligner are slightly more coverage of the palate but maintain the same thickness and material. This allows differentiated treatment possibilities depending on the cranial pattern in each patient Figure 5 a-f.
Figure 5 (a-f): Treatment plan from start, to phase 13 with pontic insertion, to the approved final plan.
The protocol calls for patients to wear the aligners while simultaneously clenching the Freedom device with one clench every three seconds, for about 30 minutes a day [6-10]. The Freedom device is designed and manufactured for the exclusive combination with this type of aligner. Recruitment of basicranial, mimic and facial muscles helps transmit adaptive forces to the entire craniofacial district facilitating dentoalveolar and palatal adaptations, all crucial for a harmonious orthodontic result.
Freedom presents three distinct flexion areas, which following the patient’s cranial type and dysfunction allow selective correction of the palate. Chewing the device with aligners activates muscles such as masseters, external and internal pterygoid, and temporalis, to name only the main ones, which exert significant forces on the dental arches, especially on tooth groups (canine to canine and right and left the first premolar to the first molar). Freedom is designed to flex and allow guided, cyclic deformation of aligners, which achieve even better fitting thanks to the applied pressure. Over a thousand cases have been treated since its existence in 2019 and preliminary studies (Perrotti, et al) on 100 adult patients can induce significant palatal morphological changes. It has been shown that this protocol expands the transverse diameters at the inter-canine and inter-molar levels, as well as increases the length of the arch, allowing for more space to align teeth [11-15].
A cyclic force system is thus realized, which has been widely shown to be the most active type of force at the sutural level. It has been found that the Freedom device should only be chewed actively by patients without painful TMJ disorders, for whom simply closing their mouth while wearing the device between the aligners is enough.
Systems that surgically intervene with screws for example exert very high and constant forces limited to the areas of implantation of the screws themselves. OP System may activate many cranial and facial muscles affecting extensive cranial areas (since tendon and connective tissue insertions are at a distance) inducing overall cranial adaptations, further studies are needed regarding this correlation. Adaptations could consist of reciprocal angular changes between many cranial bone elements. With this protocol, the premaxilla has been confirmed to achieve transverse movements in many cases of meso-brachifacial adults, while in the dolichofacial there is more availability for vertical movements.
Diagnosis
The patient was 31 years old when the treatment started and presented as follows (Figures 1,2):
- Missing tooth 13 (due to the previous extraction),
- Asymmetrical sectoral palate contraction and consequent median and premaxilla rotation,
- Skeletal Class I,
- The discrepancy between dental median and facial median with deviated nasal bones,
- Deviated asymmetric nasal cavities (following the premaxilla asymmetry),
- Brachycephalic skull.
Treatment objectives and treatment plan
An important aspect of the present case is the preimplant preparation of the space corresponding to 13. Sufficient space was obtained at the tooth and root level for proper implant placement [11-15]. Root tipping accompanied by vertical masticatory stimuli (not only orthodontic lateral displacements) was generated, made possible by the Op System protocol involving the use of the Freedom device for 30 minutes daily (Figure 4), associated with a planned pontic element placed rigidly within the aligners (Figure 3 a-c).
Case planning with the OP System protocol involves careful analysis of palatal asymmetries based on which each orthodontic correction is designed. The aligners dedicated to the Op System protocol possess a specific aligner design with lingual pins and reinforced areas (Figure 3) that integrates with the use of the Freedom myofunctional device (Figure 4). Clenching Freedom in a repetitive manner for 30 minutes a day while wearing aligners results in the combination of two distinct forces:
- Orthodontic, via the aligners which apply light and constant forces.
- Functional, via the muscle contraction unloading onto the arches (within the aligners), resulting in dentoalveolar adaptations as well as the adoption of new cranial adaptive patterns.
In the search for volumes that are in a balanced right-left relationship with each other, we ruled out sequential distalization, favoring the dynamization of the premaxilla and the entire palate. This kind of planning allows selective, functional, and dynamic management of the different palatal areas [16-20].
The patient in question at 15 years old underwent iatrogenic extraction of a key element of facial harmony: the right upper permanent canine had been extracted. Craniofacial development then proceeded in time in the absence of a morphogenic stimulus that is fundamental not only for occlusion, where residual space induces contiguous elements to migrate but mainly because the lack of transmission of canine root vector leads the entire corresponding hemi-palate to contraction at the level of the median sector of the maxillary because of the lack of developing canine draft and; the volumes and smile mimicry adapt accordingly in resultant strong asymmetry.
Thus, the therapeutic goal is to regain lost volume by balancing the hemi-palates as well as the arches, regain the correct midline, and allow the maintenance of bone thicknesses congruous with prosthetic rehabilitation in the canine area, all while respecting correct proportions.
Treatment progress
After objective craniometric and palatal evaluations, the case was programmed with the Nuvola Op System protocol; a total of 38 pairs of aligners were then planned. The patient used them according to protocol, changing them every ten days, while Freedom biting exercises took place daily.
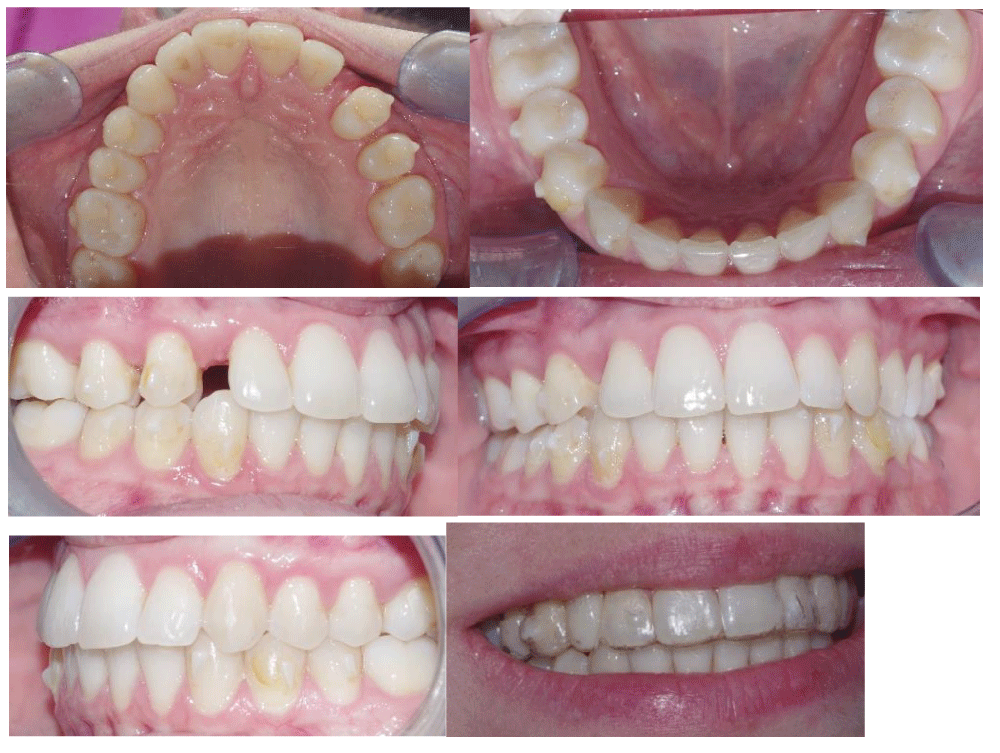
After the twelfth aligner step, the resin pontic element was created in position 13 and rigidly connected to the aligner, with an effective interproximal contact (Figure 6f). The combination with the use of Freedom also opens the space in position 13 with minimal coronal tipping of its contiguous elements due to the bodily movement of the elements [21-25].
Figure 6 (a-f): Mid-treatment intraoral photographs orthodontic treatment. The last photo shows the pontic in the aligner replacing element 13.
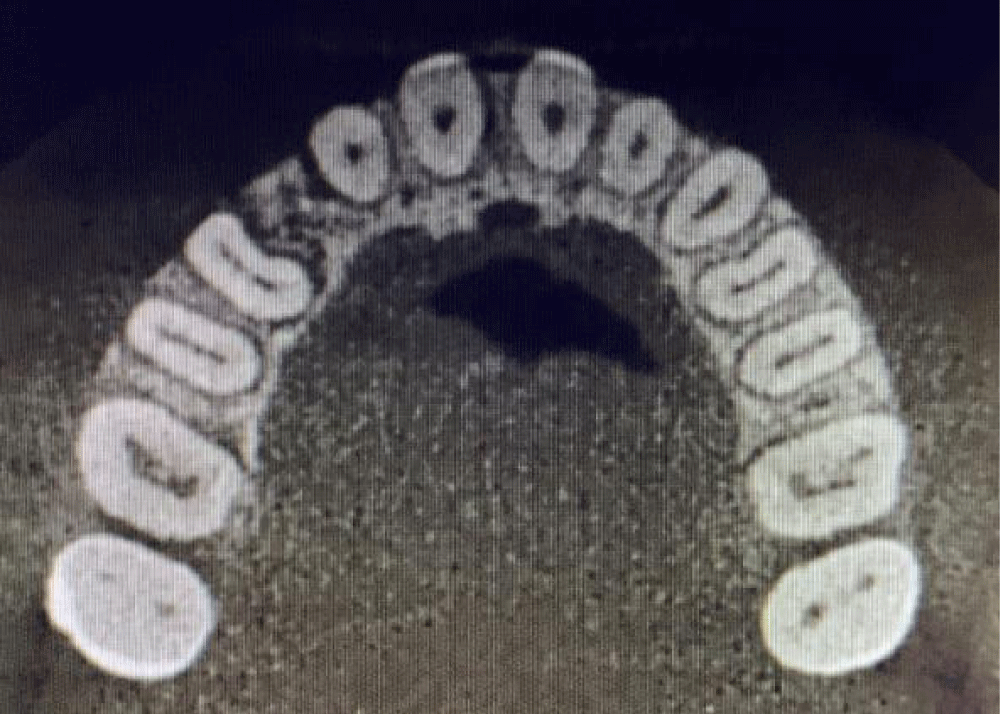
After a total of 38 aligners, of which the last 26 upper aligners presented the pontic, the patient was pleased with the results. At this point, a CT scan was performed and established there was an optimal bone presence for the team’s surgeon to place an implant (Figure 7). A temporary Maryland was placed in the 13 areas (Figure 8a). The space given to the prosthetic element is harmonious to the whole and mirrored to the contralateral (Figure 10 a,b).
Figure 7: CT slice of the upper arch after orthodontic treatment.
Figure 9: Final facial photograph.
Figure 10(a,b): The frontal photographs with the smile’s harmonic proportions.
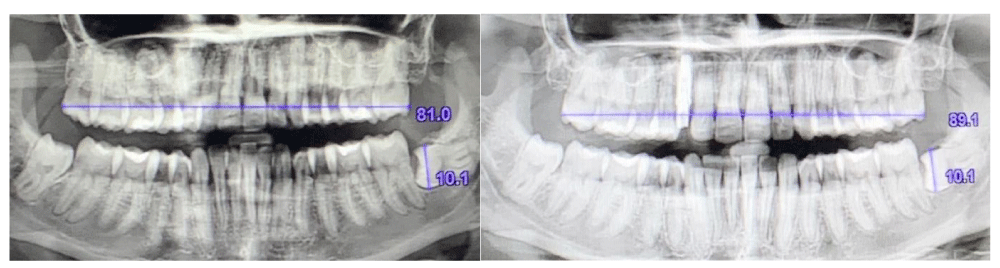
Figure 11 (a,b): Panoramic radiograph before orthodontic treatment, and after orthodontic treatment and implant placement.
After the treatment with the OP System protocol by Nuvola, the dental midline is consistent with the facial median (Figure 9). Also, Figure 11 a,b show the proportions between the ratios of the upper and lower arches before and after the therapy and the growth of the upper arch after the end of the aligner and myofunctional therapy [25-30]. The smile has effectively taken on greater volumes in mimicry and structure, especially on the right, compared to the initial situation (Figure 10 a,b).
The Nuvola® OP System protocol was effective in obtaining dental expansion in the adult patient.
A follow-up visit after 1 year shows the stability of results.
In cases where it is important to recover transverse space, the adaptive alveolar and cranial contribution can resolve otherwise difficult situations. Our treatment choice was to adopt the Op System protocol in an attempt to involve the dental, facial muscular, and basicranial aspects allowing a physiological and functional sectorial expansion of the palate and premaxilla, allowing an easy implant rehabilitation. This case report shows a successful case history of the OP System protocol in creating an excellent facial and dental esthetic as well as a functional result. The system should be evaluated over the long term to assess the stability of changes. We are therefore legitimized to adopt this protocol with increasing confidence in our future cases.
Ultimately we believe that although the sensitivity of sutures and cranial adaptations to cyclic forces is known, until now it was technically difficult to exploit this biological feature, in orthopedics and orthodontics; today with the Op System protocol it is relatively simple and noninvasive, and deserves further study.
- Rosa M. Early treatment of Class III malocclusion by RME and face-mask therapy with deciduous dentition anchorage. EJCO. 2013.
- Cephalometric changes after headgear anchored to the deciduous second molars in the early mixed dentition. Eur J Paediatr Dent. 2012; 13:176-180.
- Altiéri M. Cranial biomechanics and pathology in etiopathy. SA Geneva: Etiosciences, 1984.
- Bergersen EO. The eruption guidance myofunctional appliances: how it works, how to use it. Funct Orthod. 1984 Sep-Oct;1(3):28-9, 31-5. PMID: 6593284.
- Autet B. The rotator test; updating and new data. 3rd CEOPS Symposium. Montpellier. 2022.
- Camporesi M, Franchi L, Doldo T, Defraia E. Evaluation of mechanical properties of three different screws for rapid maxillary expansion. Biomed Eng Online. 2013 Dec 11;12:128. doi: 10.1186/1475-925X-12-128. PMID: 24330632; PMCID: PMC3880096.
- Carrafiello AA, Besi D, Giannelli L, Carrafiello L. Fondamenti di equibridonzia (OP system) ed OPmed. 2017.
- Carrafiello A. Guia a la ortodóncia postural. OP ediciones. Bogotà, 2017.
- Čirgić E, Kjellberg H, Hansen K. Treatment of large overjet in Angle Class II: division 1 malocclusion with Andresen activators versus prefabricated functional appliances-a multicenter, randomized, controlled trial. Eur J Orthod. 2016 Oct;38(5):516-24. doi: 10.1093/ejo/cjv080. Epub 2015 Nov 4. PMID: 26543061.
- Cozza P, Ballanti F. Analisi cefalometrica e diagnosi ortodontica. Società Editrice Universo, 2004.
- Pacioli L, Leonardo V, De divina proportione, 1509. Leopold Publishing, 2014.
- Deshayes MJ. L'art de traiter avant 6 ans. Cranexplo, 2006.
- Farronato G, Maspero C, Farronato D. Orthodontic movement of a dilacerated maxillary incisor in mixed dentition treatment. Dent Traumatol. 2009 Aug;25(4):451-6. doi: 10.1111/j.1600-9657.2008.00722.x. Epub 2009 Jun 10. PMID: 19519865.
- Susanibar F, Parra D, Dioses A. Motricidad orofacial. Fundamentos basados en evidencias. Volumen I. GIUNTIEOS Psychometrics SL, 2015.
- Stefanelli G. Sistema stomatognatico nel contesto posturale. Edizione Ermes, 2003.
- Idris G, Hajeer MY, Al-Jundi A. Soft- and hard-tissue changes following treatment of Class II division 1 malocclusion with Activator versus Trainer: a randomized controlled trial. Eur J Orthod. 2019 Jan 23;41(1):21-28. doi: 10.1093/ejo/cjy014. PMID: 29617755.
- Maspero C, Farronato G. Metodica di espansione palatale. Revisione della Letteratura: basi biologiche. Parte I. 2009. Ortodonzia Clinica.
- Mao JJ. Mechanobiology of craniofacial sutures. J Dent Res. 2002 Dec;81(12):810-6. doi: 10.1177/154405910208101203. PMID: 12454093.
- Clauzade M, Marty JP. Orto posturodonzia 2. Roma: Marrapese Editore, 2008. Ortoposturodonzia. 1: 2004.
- Nerio P, Ortognatodonzia A, Ortodontotecnica nell’epoca della dentizione mista. Edizioni Martina, 2008.
- Oberheim MC, Mao JJ. Bone strain patterns of the zygomatic complex in response to simulated orthopedic forces. J Dent Res. 2002 Sep;81(9):608-12. doi: 10.1177/154405910208100906. PMID: 12202641.
- Perrotti G, Carrafiello A, Rossi O, Karanxha L, Baccaglione G, Del Fabbro M. Clinical Use of Aligners Associated with Nuvola® OP System for Transverse Maxillary Deficiency: A Retrospective Study on 100 Patients. Int J Environ Res Public Health. 2022 May 9;19(9):5751. doi: 10.3390/ijerph19095751. PMID: 35565146; PMCID: PMC9103427.
- Perrotti G, De Vecchi L, Testori T, Weinstein RL. Proposta di analisi cefalometrica 3D per una analisi facciale globale in ortodonzia e implantologia. Italian Oral Surgery. 2012; 11(5):s154-164.
- Zecca PA, Fastuca R, Beretta M, Caprioglio A, Macchi A. Correlation Assessment between Three-Dimensional Facial Soft Tissue Scan and Lateral Cephalometric Radiography in Orthodontic Diagnosis. Int J Dent. 2016;2016:1473918. doi: 10.1155/2016/1473918. Epub 2016 May 29. PMID: 27313615; PMCID: PMC4903122.
- Shibusawa N, Endo Y, Morimoto N, Takahashi I, Miura T. Mathematical modeling of palatal suture pattern formation: morphological differences between sagittal and palatal sutures. Sci Rep. 2021 Apr 26;11(1):8995. doi: 10.1038/s41598-021-88255-y. PMID: 33903631; PMCID: PMC8076228.
- Stefanelli G. Craniodonzia. Il sistema ALF. Nike (Ortobello), 2011.
- Tepedino M, Chimenti C, Masedu F, Iancu Potrubacz M. Predictable method to deliver physiologic force for extrusion of palatally impacted maxillary canines. Am J Orthod Dentofacial Orthop. 2018 Feb;153(2):195-203. doi: 10.1016/j.ajodo.2017.05.035. PMID: 29407496.
- Vij K, Mao JJ. Geometry and cell density of rat craniofacial sutures during early postnatal development and upon in vivo cyclic loading. Bone. 2006 May;38(5):722-30. doi: 10.1016/j.bone.2005.10.028. Epub 2006 Jan 18. PMID: 16413234.
- Wishney M, Darendeliler MA, Dalci O. Myofunctional therapy and prefabricated functional appliances: an overview of the history and evidence. Aust Dent J. 2019 Jun;64(2):135-144. doi: 10.1111/adj.12690. Epub 2019 Apr 29. PMID: 30921479.