More Information
Submitted: November 29, 2023 | Approved: December 18, 2023 | Published: December 19, 2023
How to cite this article: Ettore E, Maria P, Nunziata C, Pietro A. Success, Survival and Prognostic Factors in Implant Prosthesis: Experimental Study. J Oral Health Craniofac Sci. 2023; 7: 024-028.
DOI: 10.29328/journal.johcs.1001045
Copyright License: © 2023 Ettore E, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Implants; Success; Survival rate; Dental prosthesis
Success, Survival and Prognostic Factors in Implant Prosthesis: Experimental Study
Epifania Ettore* , Pietrantonio Maria, Christian Nunziata and Ausiello Pietro
, Pietrantonio Maria, Christian Nunziata and Ausiello Pietro
Department of Neurosciences, Reproductive and Odontostomatological Sciences, University of Naples Federico II, Naples, Italy
*Address for Correspondence: Epifania Ettore, Professor, Department of Neurosciences, Reproductive and Odontostomatological Sciences, University of Naples Federico II, Via Pansini, n.5 80100, Naples, Italy, Email: [email protected]
The primary objective of this study was to detect the success and short-term survival rate of dental implant prosthetic therapy.
The valuation of a possible relationship between the general and local clinical conditions of the patients (presence of risk factors and type of dental implant-supported prosthesis) and the satisfaction perceived by the patient, with success and survival of implant devices was investigated.
The sample trial consisted of 23 patients, for a total of 50 dental implants supporting a prosthetic therapy. Preliminarily, an analysis of averages and frequencies of the anamnestic data was presented, as numbers and percentages. The implant success rate was calculated by assessing whether the implants fulfilled the success criteria defined by the Pisa Consensus Conference. The ANOVA test was used to check whether there was an association between the success of the implant device, the anamnestic data collected, and the type of prosthesis supported by the implants. Finally, the survival rate was calculated using the Kaplan - Meier method.
The 2-year success rate of 50 implants was assessed at 98%. The 2-year survival rate was 97%. Finally, sex, age, compensated diabetes, a smaller and equal number of cigarettes per day (10 per day), the BOP, and the type of titanium dental implants supported by prosthesis, do not determine a change in success and are therefore not adequate parameters to predict the outcome of implant success. Following the results obtained, it is appropriate to continue the research by expanding the clinical observation times in order to obtain more solid scientific and clinical evidence.
Brånemark, et al. [1], first published the first long-term longitudinal study of endosseous dental titanium implants in 1977 and they showed it was possible to obtain direct bone apposition on the implant surfaces in humans. Albrektsson, et al. [2] in 1991 defined osseointegration as “A process in which a clinically asymptomatic rigid fixation of the alloplastic material in the bone is obtained during the functional load”. Today, titanium dental implants turn out to be a constant and predictable approach in fixed prosthetic rehabilitations both in cases of partial and total edentulism in humans.
The principle of implant prosthetic therapy is based on this concept of osseointegration and consists of inserting the dental titanium implants in the bone and maintaining their stability over time even when the implants are subjected to the functional load. Several studies have determined the validity of these devices [3] and recommended clinical protocols to standardize the operative procedure and improve the expectedness of the results [4].
The use of osseo-integrated dental titanium implants is nowadays one of the most widespread and predictable methods for partial or total dental prosthetic rehabilitation. The growing expectations of the patient both from an aesthetic and functional point of view have meant that implantology is now a widely used practice in dentistry [5]. It allows, on the one hand, to guarantee fixed rehabilitations to edentulous patients and, on the other, not to compromise the natural dentition.
In recent years, numerous studies have been carried out to obtain a titanium dental implant that is as performing as possible and that allows optimal bone tissue anchoring. For this reason, different titanium implant surfaces, connections, and shapes have been introduced in reason of the prosthetic load times and the surgical techniques used. These have conveniently changed, in the time [6].
For these reasons, there are numerous dental implants on the market that differ in surface area, connection, and shape [7].
Therefore, the objective of the study was to detect the success rate and the short-term survival rate of implant-prosthetic therapy (Dura-vit, B&B Dental Implant company, Bologna, Italy). Moreover, we set as a secondary objective assessment a possible association between the general and local clinical condition of the patient (presence of risk factors and type of implant-borne restorations) with the success and survival of the implant devices.
A trial of 23 patients was analyzed for a total of 50 dental implants. The study also received the approval of the ethics committee of the University of Napoli Federico II: Protocol number 311/18.
The Dura-vit conexa (B&B Dental implant, Bologna, Italy) has variable threads and a tapered design for accurate implant placement, self-drilling, conexa connection (morse-type), improved esthetics, and better load distribution. It features a special round-shaped apex that pushes the bone graft and it has a built-in platform switching.
Patient selection
The selection of patients was of fundamental importance since it allowed to exclude all those subjects whose intrinsic conditions, such as the general or extrinsic state of health, such as taking medicines or smoking could have affected the outcome of the treatment.
In this regard, it was necessary to proceed to a careful analysis of the patient’s remote and proximate anamnesis and the pharmacological therapies assumed. As well as the motivation and assessment of patient expectations.
Inclusion criteria: Only patients undergoing implant-prosthetic therapy for partial or total edentulism were included in the study, informed of the procedures, and willing to cooperate and follow the instructions given by the clinicians.
Exclusion criteria: All subjects with general and local conditions were excluded from the study, which turned out to be contraindications to implant placement. Then:
- Presence of general absolute contraindications (recent ischemic heart disease; immune deficiency; severe platelet diseases and coagulopathies; severe nephropathy; severe liver disease; therapy with bisphosphonates; radiant therapies in the head and neck district);
- Presence of general relative contraindications (age below 18; smoking> 10 cigarettes per day; non-compensated diabetes, periodontal disease);
- Presence of local contraindications (serious stomatopathies; drug gingivopathies; maxillary osteopathies; tumors of hard or soft tissues of the oral cavity; absence of enough bone size; insufficient oral hygiene; aggressive periodontitis in active phase).
Evaluation of implant status
In a preliminary phase of the study, a careful investigation of the present literature was carried out regarding the most reliable and certified methods for the evaluation of implant success.
In 1986, Albrektsson, et al. [3] defined some clinical and radiographic parameters that, in the presence of implants inserted in the oral cavity and prosthetically rehabilitated, had to be realized in order to be able to talk about success. These parameters were modified in 2007 by the Consensus Conference held in Pisa [8], during which they were defined as clinical indices for the evaluation of success:
- Pain;
- Mobility;
- Radiographic Crestal Bone Loss;
- Probing Depths;
- Peri-implant disease.
Furthermore, 4 categories were distinguished: 1) success, 2) satisfactory survival, 3) compromised survival, and 4) failure (Table 1).
| Table 1: Health scale for dental implants. | |
| Implant Quality scale group | Clinical Conditions |
|
|
|
|
|
|
|
Any of following:
|
Therefore, during each planned recall, clinical and radiographic data and values were collected, concerning the indexes described above; in order to assess whether the plants covered by the study met the criteria, that define a plant as a success, according to the Consensus Conference of Pisa.
Operational phases
The first step included, first of all, information and consent from the recruited subjects for participation in the study and processing of personal data; the collection of anamnestic data such as age, sex, presence of compensated diabetes, smoking (number of cigarettes/day), oral hygiene (BOP), number of implants present per patient and the type of prosthesis (single crown, bridge, full arch, toronto bridge). Secondly, at 3, 6, 12, and 24 months from implant placement, pain, mobility, radiographic crestal bone loss, bleeding on probe (BOP), and suppuration, stability, and efficiency of prosthetic rehabilitation were evaluated [9].
Statistical analysis of data
At the end of the operational phases, all the data collected were first analyzed using the IBM SPSS statistical software. Preliminarily, an analysis of the mean and frequency of the anamnestic data was presented, as number and percentage. The implant success rate was calculated by assessing whether the implants fulfilled the success criteria defined by the Pisa Consensus Conference (absence of pain, lack of mobility, radiographic bone loss < 2 mm from the initial operation, absence of infection history) [7,10].
The univariate variance test (ANOVA) was used to verify if there is an association between the success of the implant device, the anamnestic data detected, and the type of implant-supported prosthesis. Finally, the survival rate was calculated using the Kaplan - Meier method.
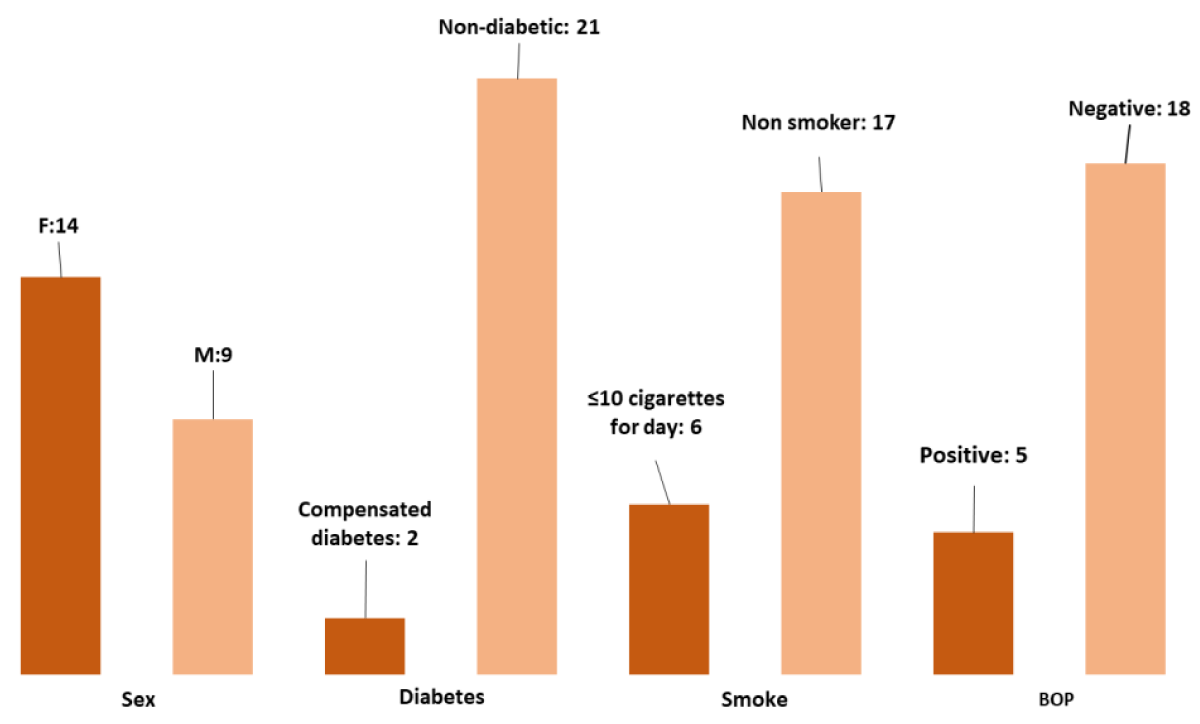
Of 23 patients, for a total of 50 implants. The patients’ ages are between 38 and 67; of which 14 are women (61%) and 9 are male (39%). Two patients had compensated diabetes (9%); while six smoked a number of ≤ 10/day (30%) and finally, five patients had positive bleeding on probe (BOP) (22%) (Table 2).
Table 2: Distribution: Sex, diabetes, smoke, and BOP.
The number of implants present in the various patients ranged from a minimum of 1 to a maximum of 12, as specified in (Table 3) as well as the type of prosthesis. The variability of the type of prosthesis is remarkable, we find the presence of single crowns, bridges, bridges with mixed support, full arch with mixed support, and toronto bridge [11].
| Table 3: Number of implants for patients. | |
| Number of implants for patient | Number of patients |
| 1 | 9 |
| 2 | 10 |
| 3 | 3 |
| 12 | 1 |
In order to assess success, satisfactory survival, impaired survival, and failure at 3, 6, 12, and 24 months, pain, mobility, radiographic bone loss, bleeding on probe, and suppuration were evaluated (Table 4).
| Table 4: Evaluation of pain, mobility, bone loss assessed Rx, and bleeding on probe (BOP) at 3, 6, 12 and 24 months. | ||||
| Pain | Mobility | Radiographic bone loss | Bleeding on probe (BOP) | |
| t = 3 months | Absent | Absent* | 0* | Negative |
| t = 6 months | Absent | Absent | 0 | Negative |
| t = 12 months | Absent | Absent | 0,1 | Negative |
| t = 24 months | Absent** | Absent** | 0,1 - 0,14 ** | Negative** |
| *with the exception of 1 implant that presented: mobility, bone loss > half of the implant and suppuration. **with the exception of 1 implant that presented: pain, mobility, bone loss > half of the implant and suppuration. |
||||
At 3 months, 49 implants showed an absence of pain, absence of mobility, absence of radiographic bone loss, absence of bleeding on the probe, and absence of suppuration. Only one implant presented: mobility, radiographic bone loss> half of the implant, and suppuration. The patient, whose implant had been lost, was not a diabetic, did not smoke, had a positive BOP, and the type of prosthesis that should have supported the failed implant, was a ceramic metal crown [12].
After 3 months, the implants were loaded and the subsequent check, this time after loading, was carried out at 6 months. On this occasion the 49 plants respected all the success criteria defined by the Pisa Consensus Conference.
At 12 months, bone resorption was observed on average around 0.1 mm. While the pain, mobility, and history of infection were absent.
At 24 months, the parameters analyzed for 48 implants were in line with those measured at 12 months, except for bone loss which was on average between 0.1 and 0.14 mm. Only one implant presented: pain, mobility, radiographic bone loss> half of the implant, and suppuration.
The patient, whose implant had been lost, was not a diabetic, smoked a number of cigarettes less than or equal to 10 per day, had a negative BOP and the type of prosthesis supported by the failed implant was a single crown.
Therefore, with reference to the success criteria introduced in 2007 by the Consensus Conference of Pisa, of the 50 implants under study, two implants had failed and 48 were compliant with the success criteria, so the success rate was 98%.
Repeated analysis of the univariate variance test (ANOVA) between the various anamnestic factors considered in the study and success showed that sex, age, compensated diabetes, the number of cigarettes ≤ 10/day, the BOP, and the type of implants supported by implants, do not determine a change in success and therefore aren’t adequate parameters to predict, the outcome of implant success as shown in Table 5.
| Table 5: Results of ANOVA. | ||
| Parameters | F | p Value |
| Sex | 0,3 | 0,587 |
| Age | 0,508 | 0,48 |
| Diabetes compensated | 0,274 | 0,603 |
| Number of cigarettes ≤ 10/day | 1,152 | 0,288 |
| BOP | 2,254 | 0,14 |
| Type of prosthesis | 2,537 | 0,118 |
The survival rate was calculated using the Kaplan method– Meier, by which a cumulative 24-month survival of 97% was detected (Table 6).
| Table 6: Survival rate results by Kaplan - Meier method. | |||||||
| Time | At risk | Failed | Survival | Censored | Instant mortality | Survival in the period | Cumulative survival |
| 3 | 50 | 1 | 49 | 0 | 0,02 | 0,98 | 0,98 |
| 6 | 49 | 0 | 49 | 0 | 0 | 1 | 0,98 |
| 12 | 49 | 0 | 49 | 0 | 0 | 1 | 0,98 |
| 24 | 49 | 1 | 48 | 0 | 0,0240816 | 0,97959184 | 0,97 |
The aim of this retrospective study was to determine the success and survival rate of 50 plants at two years; aimed at evaluating a possible association between the anamnestic factors and type of implants supported by implants, with the success and survival of implant devices.
The success was evaluated by reference to the criteria expressed by the ICOI Pisa Consensus Conference in 2007, according to which 48 implants were successful, while two implants failed. Reporting, therefore, a success rate of 98%.
Of the two failed implants, one was lost at the first follow-up at three months and the second at 24 months. The patient, whose implant had been lost after 3 months, was not a diabetic, did not smoke, had a positive BOP and the type of prosthesis that should have supported the failed implant was a bridge. In this case, we talk about early failure, since it occurred before loading.
Specifically, the osseointegration process had not occurred and the mechanisms that normally lead to healing by bone apposition did not take place. Probably, this occurs because of an excessive space between the surface of the implant and the bone tissue, with consequent interposition of fibrous tissue at the interface. Another explanation, it could be dependent on the use of an aggressive surgical technique preparation of the implant-bone site with overheating of the bone itself reaching a temperature above 47 °C. An early bone site infection or poor quality and quantity of bone have been also described as secondary causes [13].
The second patient, whose implant had failed at 24 months, was not a diabetic, smoked a number of cigarettes ≤ 10/day, had a negative BOP and the type of prosthesis supported by the failed implant was a single crown. In this case, failure is defined as late because it occurs after osseointegration and it’s probably mechanical, so it results from a traumatic mechanism of the occlusal forces.
Instead, cumulative 2-year survival was 97%, thus consistent with the literature.
Through the analysis of univariate variance (ANOVA) it was possible to verify that sex, age, diabetes compensated, the number of cigarettes less than or equal to 10 per day, BOP, and the type of prosthesis supported by implants, do not determine a change in success and are therefore not adequate parameters to predict, the outcome of implant success. However, in relation to sex, there are studies from which emerge an association between the male sex and implant failure [14].
As for the condition in which patients appear to have a form of compensated diabetes, what emerged from our study, is that this condition does not alter implant success; and this is in agreement with other results published in the literature [9,15].
Data analysis has shown that there is no statistically significant correlation between success and mild smoking (≤ 10 cigarettes per day), which is not different from what has already been stated in other studies. According to this, the success rate of dental implants is compromised in heavy smokers. In particular, long-term studies have shown that the effect of smoking appears to be dose-dependent, with noticeably higher levels of disease progression in heavy smokers (> 10 cigarettes per day) [16] and with success differences between light smokers and heavy smokers, with percentages for light smokers close to those of non-smokers [6].
Another interesting fact is the absence of a correlation between the type of prosthesis and implant success. Therefore, the choice of the type of prosthesis cannot be considered a predictive fact of success, or less, implant.
In conclusion, considering as successful the condition defined by the Pisa Consensus Conference, the 2-year success rate of 50 implants was 98%. The survival rate calculated using the Kaplan-Meier method, at two years, was 97%.
Finally, sex, age, compensated diabetes, the number of cigarettes ≤10/day, the BOP, and the type of implants supported by implants do not determine a change in success and are therefore not adequate parameters to predict the outcome of implant success.
Following the results obtained from this study, it is appropriate to continue the research by expanding the clinical observation times in order to obtain more solid scientific evidence in agreement with international literature.
- Brånemark PI, Hansson BO, Adell R, Breine U, Lindström J, Hallén O, Ohman A. Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-year period. Scand J Plast Reconstr Surg Suppl. 1977;16:1-132. PMID: 356184.
- Zarb GA, Albrektsson T. Osseointegation – a requiem for the periodontal ligament?. Int J Periodontics Restorative Dent. 1991; 11 (1):88-91
- Duong HY, Roccuzzo A, Stähli A, Salvi GE, Lang NP, Sculean A. Oral health-related quality of life of patients rehabilitated with fixed and removable implant-supported dental prostheses. Periodontol 2000. 2022 Feb;88(1):201-237. doi: 10.1111/prd.12419. PMID: 35103325; PMCID: PMC9304161.
- Bolzoni A, D'Orto O, Laganà F, Avvantaggiato P, Candotto V. Survival and success rate of spiral implants inserted mandible. J Biol Regul Homeost Agents. 2020 Jan-Feb;34(1 Suppl. 2):7-11. DENTAL SUPPLEMENT. PMID: 32270662.
- Ormianer Z, Block J, Matalon S, Kohen J. The Effect of Moderately Controlled Type 2 Diabetes on Dental Implant Survival and Peri-implant Bone Loss: A Long-Term Retrospective Study. Int J Oral Maxillofac Implants. 2018 Mar/Apr;33(2):389-394. doi: 10.11607/jomi.5838. PMID: 29534127.
- Klotz AL, Fobbe H, Rammelsberg P, Lorenzo Bermejo J, Kappel S. Survival and success of tooth-implant-supported and solely implant-supported double-crown-retained overdentures: A prospective study over a period of up to 11 years. Clin Oral Implants Res. 2021 Dec;32(12):1425-1432. doi: 10.1111/clr.13842. Epub 2021 Oct 29. PMID: 34543479.
- Tonetti MS. Cigarette smoking and periodontal diseases: etiology and management of disease. Ann Periodontol. 1998 Jul;3(1):88-101. doi: 10.1902/annals.1998.3.1.88. PMID: 9722693.
- Albrektsson T, Zarb G, Worthington P, Eriksson AR. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986 Summer;1(1):11-25. PMID: 3527955.
- Rameh S, Menhall A, Younes R. Key factors influencing short implant success. Oral Maxillofac Surg. 2020 Sep;24(3):263-275. doi: 10.1007/s10006-020-00841-y. Epub 2020 Apr 23. PMID: 32323043.
- Epifania E, Sanzullo R, Sorrentino R, Ausiello P. Evaluation of Satisfaction Perceived by Prosthetic Patients Compared to Clinical and Technical Variables. J Int Soc Prev Community Dent. 2018 May-Jun;8(3):252-258. doi: 10.4103/jispcd.JISPCD_27_18. Epub 2018 May 17. PMID: 29911064; PMCID: PMC5985683.
- Tribst JPM, Dal Piva AMO, Lo Giudice R, Borges ALS, Bottino MA, Epifania E, Ausiello P. The Influence of Custom-Milled Framework Design for an Implant-Supported Full-Arch Fixed Dental Prosthesis: 3D-FEA Sudy. Int J Environ Res Public Health. 2020 Jun 5;17(11):4040. doi: 10.3390/ijerph17114040. PMID: 32517097; PMCID: PMC7313457.
- Epifania E, di Lauro AE, Ausiello P, Mancone A, Garcia-Godoy F, Mendes Tribst JP. Effect of crown stiffness and prosthetic screw absence on the stress distribution in implant-supported restoration: A 3D finite element analysis. PLoS One. 2023 May 5;18(5):e0285421. doi: 10.1371/journal.pone.0285421. PMID: 37146083; PMCID: PMC10162567.
- Misch CE, Perel ML, Wang HL, Sammartino G, Galindo-Moreno P, Trisi P, Steigmann M, Rebaudi A, Palti A, Pikos MA, Schwartz-Arad D, Choukroun J, Gutierrez-Perez JL, Marenzi G, Valavanis DK. Implant success, survival, and failure: the International Congress of Oral Implantologists (ICOI) Pisa Consensus Conference. Implant Dent. 2008 Mar;17(1):5-15. doi: 10.1097/ID.0b013e3181676059. PMID: 18332753.
- Quirynen M, De Soete M, van Steenberghe D. Infectious risks for oral implants: a review of the literature. Clin Oral Implants Res. 2002 Feb;13(1):1-19. doi: 10.1034/j.1600-0501.2002.130101.x. PMID: 12005139.
- Grisar K, Sinha D, Schoenaers J, Dormaar T, Politis C. Retrospective Analysis of Dental Implants Placed Between 2012 and 2014: Indications, Risk Factors, and Early Survival. Int J Oral Maxillofac Implants. 2017 May/June;32(3):649–654. doi: 10.11607/jomi.5332. Epub 2017 Feb 17. PMID: 28212455.
- Brignardello-Petersen R. No evidence of higher rates of implant failure in people with controlled diabetes. J Am Dent Assoc. 2017 Apr;148(4):e5. doi: 10.1016/j.adaj.2016.11.026. Epub 2017 Jan 11. PMID: 28088264.