More Information
Submitted: February 01, 2024 | Approved: February 20, 2024 | Published: February 21, 2024
How to cite this article: Khachatryan H, Boshnaghyan E, Papoyan S, Hakobyan G. Hygiene and Care Protocols for Implant-supported Dental Prostheses in Patients with Diabetes. J Oral Health Craniofac Sci. 2024; 9: 009-014.
DOI: 10.29328/journal.johcs.1001047
Copyright License: © 2024 Khachatryan H, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Periodontitis; Dental implant; Prosthodontic; Maintenance protocols
Hygiene and Care Protocols for Implant-supported Dental Prostheses in Patients with Diabetes
Hakob Khachatryan1, Emma Boshnaghyan2, Sevak Papoyan3 and Gagik Hakobyan4*
1Central Clinical Military Hospital (Ministry of Defence of the Republic of Armenia), Yerevan State Medical University after M. Heratsi, Yerevan, Armenia
2Meher Babian Dental Office, General Dentistry, 1111 S. Glendale, California, USA
3Yerevan State Medical University after M. Heratsi, Yerevan, Armenia
4Professor, Head of Department of Oral and Maxillofacial Surgery, Yerevan State Medical University after M. Heratsi, Yerevan, Armenia
*Address for Correspondence: Gagik Hakobyan, Professor, Head of the Department of Oral and Maxillofacial Surgery, Yerevan State Medical University, Yerevan, Armenia, Email: [email protected]
Background: Prophylactic dental procedures following implant placement are critical to the long-term success of implants and are also dependent on the patient maintaining effective home care.
Purpose: Evaluation of the effectiveness of preventive measures in patients with diabetes during long periods after prosthetic treatment with implants.
Materials and methods: The study included 62 patients with diabetes with edentulism using 146 dental implants. Patients underwent constant monitoring, including regular occupational hygiene during follow-up examinations. Their frequency was set individually from 2 to 4 times A clinical index including Bleeding on Probing (BOP), Probing Depth (PD), and Marginal Bone Loss (MBL).
Results: In patients included in the preventive protocol after 12 months, the mean BOP was 1.4 ± 0.15, and PPD was 2.46 ± 0.42. After 12 months in patients mean MBL was 0.72 ± 0.6 mm, after 3 years MBL was 1.24 ± 0.25 mm. For patients who were excluded from preventive services after 12 months, the mean BOP 1.9 ± 0.25, and the mean PPD was 3.56 ± 0.28). After 12 months in patients mean MBL was 0.87 ± 0.7 mm, after 3 years MBL was 1.52 ± 0.32 mm (p > 05). Compared to persons enrolled in the preventive protocol, those in the group without services were more likely to develop peri-implantitis (42.4% vs. 12,6%). The survival rate of implants after 3 years was 98.4%. The survival rate of implants in those patients who were excluded from preventive services after 3 years was 95.4%.
Conclusion: For patients with diabetes, regular medical examinations, accompanied by professional oral hygiene procedures, prevent the development of negative reactions of the soft tissues surrounding the implant.
Over the past decade and a half, dental implantation as a method of treating partial and complete edentulism has gained a strong position in modern prosthetic dentistry [1,2]. Dental implants for total or partially edentulous patients are an effective method of replacing natural teeth with long-term results [3-5]. Not so long ago, diabetes mellitus was a contraindication for implantation, but technology does not stand still and today such patients also have access to implant prosthetics [6-8]. Diabetes mellitus is a disease of the endocrine system in which the body lacks the pancreatic hormone insulin. Type 1 diabetes is associated with low production of the hormone, type 2 - with its insufficient absorption and poor cell sensitivity [9-11]. A direct consequence of the disease is increased blood sugar. A person feels constant thirst and hunger, loses weight, and is bothered by frequent urination. Due to high sugar content in a type II diabetic patient metabolism in all its forms is disrupted [12-14], blood vessels suffer; immunity decreases; and bones become brittle.
In type II diabetic patients tissue regeneration slows down significantly, recovery processes are going very slowly, and wounds become infected, fester and become non-healing [15-18]. Deep metabolic disorders in the body lead to serious diseases of the teeth and gums [19-21]. The salivary glands produce little saliva in diabetic patients, tooth enamel is quickly destroyed and caries develop at an accelerated rate [22,23]. With a high concentration of carbohydrates, fungal flora is activated. It multiplies easily and affects previously healthy teeth [24]. Persistent foci of chronic infection arise in the oral cavity. When care is taken incorrectly, bacteria accumulate in tooth crevices and cavities, maintaining inflammation in them [25-28].
During surgery, dentists are faced with increased bleeding from the wound. Postoperative swelling and hematomas take a long time to resolve and cause significant pain [29-31]. The healing of the implant slows down, takes several months longer, and sometimes does not occur at all in diabetics [32,33]. This was an obstacle to implantation since complications often occurred in this group of patients after surgery. Аfter extensive research it was established that dental implantation is quite possible in a compensated form of diabetes - when, against the background of constant treatment, the sugar level remains normal for 2 months - 3 months or more [34,35].
Patients with type 2 diabetes mellitus, who developed the disease more recently, tolerate implantation better and recover faster since their bone structure is more dense and the body is in good condition [36,37]. Today, an absolute contraindication for dental restoration using implants is decompensated diabetes mellitus, when the sugar level is much higher than normal and is not regulated in any way. Insulin-dependent patients and people with type 1 diabetes mellitus, who have significantly reduced bone density, which sharply increases the risk of implant failure, may also be refused [38]. Despite the fact that implantation in recent years has had a high level of success, an urgent problem in dentistry remains the possibility of long-term complications associated, first of all, with the development of inflammation of the tissues surrounding the osseointegrated implant, which can ultimately lead to the loss of the dental implants [39,40].
The etiology of implant failure is complex; among the etiological factors, it is emphasized by the colonization of the peri-implantation sulcus by specific pathogenic microorganisms, initiated by the initial stage of inflammatory processes ending in implant rejection [41,42]. Guaranteed success in servicing structures based on dental implants requires a team of specialists to carry out professional preventative procedures for the care of implants [43]. Implant health checks include probing depth, bleeding on probing, prosthetic/abutment components, implant stability, occlusion, and signs of disease activity (eg, pain) [43,44].
Various studies have published evidence that regular patient monitoring, implant care, and supportive care are key to preventing peri-implantitis in patients [45,46].
There are few articles demonstrating the value of an implant care protocol compared to implants that have been out of care for a long time and lack professional hygiene. This article discusses the importance of oral hygiene when caring for implants.
This prospective study included 62 partially or fully edentulous patients using 154 dental implants at the Department of Oral and Maxillofacial Surgery, Yerevan State Medical University, Yerevan, Armenia, between 2021 and 2023. The ages of the patients ranged between 26 and 43 years (34 males and 28 females). The study was reviewed and approved by the Ethical Committee of Yerevan State Medical (N 23 20 /03 2021) and in accordance with those of the World Medical Association and the Helsinki Declaration. Patients were informed verbally and in writing about the study and gave written informed consent.
Patients underwent a thorough clinical examination according to a generally accepted scheme. Patients after implantation were subject to constant monitoring, including regular professional hygiene during control examinations. Clinical index including; Bleeding On Probing (BOP), Probing Depth (PD), and Marginal Bone Loss (MBL) were recorded.
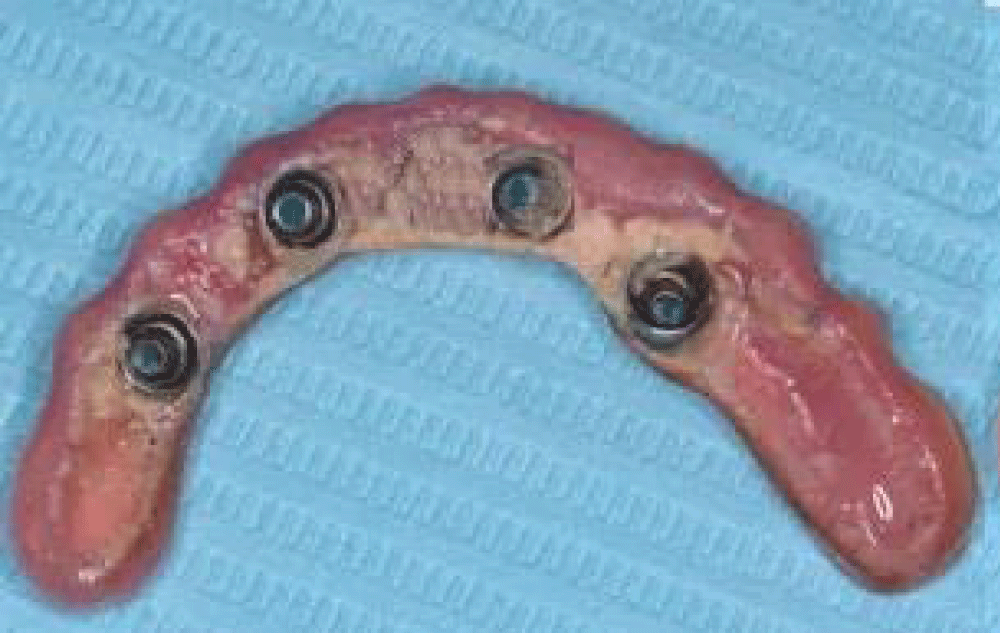
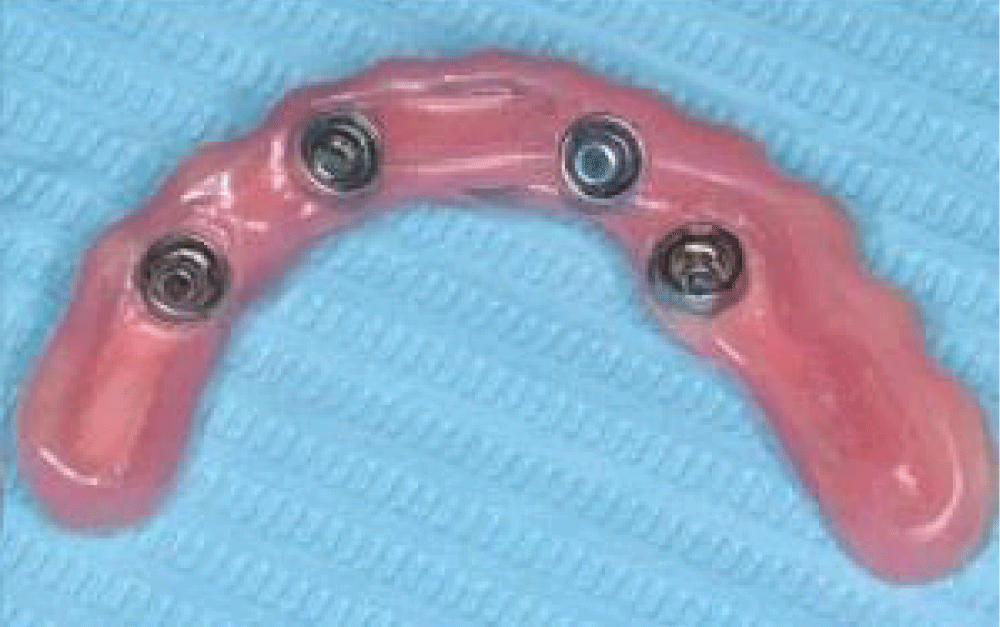
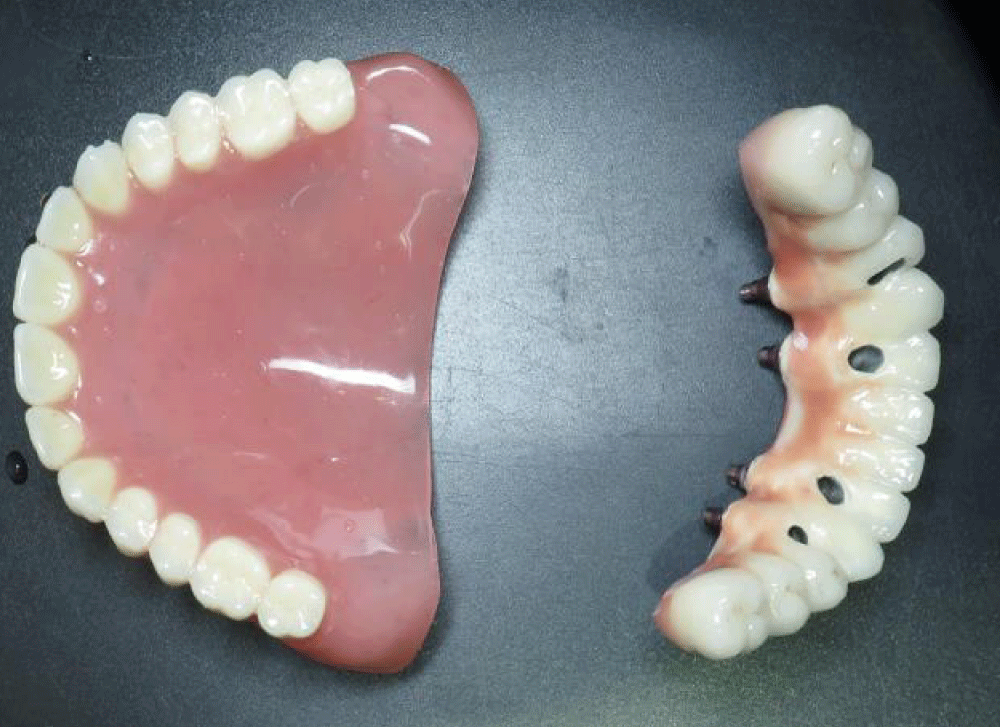
Their frequency was set individually - from 2 to 4 times. Calculus and plaque removal were performed using Steri-Oss scalers (Yorba Linda, California) made of graphite-reinforced nylon; subgingival irrigation with an antiseptic such as peroxide, Listerine or chlorhexidine using a plastic irrigation tip (Figures 1-4).
Figure 1: Before carrying out hygienic measures, calculus and plaque are observed on the removed fixed prosthetic structure screw-fixed to the lower jaw implants.
Figure 2: After removing the prosthetic structure, it is cleaned and polished.
Figure 3: Removable complete denture of the upper jaw, screw fixation of the prosthetic structure on implants of the lower jaw.
Figure 4: The patient’s oral cavity after installation of the prosthetic structure.
In the case of early-stage peri-implantitis, local application of microencapsulated minocycline (Arestin) and 0.12% chlorhexidine gel reduced the depth of pockets and bleeding during probing.
Clinical and radiographic controls were made regularly, during dynamic observation, oral hygiene and the level of plaque control were assessed; probing depth, mobility, and bleeding during probing; assessment of any mucogingival deformities; occlusion monitoring; X-ray examination. The most common signs of peri-implantation mucositis are discoloration and bleeding on probing. The criteria for implant success were assessed. Criteria for failure included: implant mobility (> 1 mm), and radiographic bone loss (> 1/3 implant height).
Statistical analysis
Statistical were carried out using SPSS (SPSS Software Company, Chicago, IL, USA). The differences between follow-up periods were tested by paired Student’s t-test, and the p-values < 0.05 were considered statistically significant.
In patients included in the preventive protocol the mean BOP after 12 months BOP 1.4 ± 0.15 (p >0.05), and PPD after 12 months was 2.46 ± 0.42. After 12 months in patients mean MBL was 0.72 ± 0.6 mm, after 3 years MBL was 1.24 ± 0.25 mm (p > 05). Clinical indicators for patients who were excluded from preventive services after 12 months mean BOP 1.9 ± 0.25 (p > 0.05), and PPD after 12 months was 3.56 ± 0.28. After 12 months in patients mean MBL was 0.87 ± 0.7 mm, after 3 years MBL was 1.52 ± 0.32 mm (p > 05).
Long-term functioning of implants requires ongoing maintenance and monitoring, which additionally includes an assessment of the patient’s general and oral health, professional implant maintenance and careful home care. Not all patients are aware that poor oral hygiene is a significant risk factor for the development of peri-implantitis mucositis, which can be reversible with early treatment, can progress to peri-implantitis, and can ultimately lead to implant loss [47-49]. In patients with implants, if there is a tendency to inflammation of the tissues around the implants, daily home cleaning with chemotherapeutic agents in the form of rinsing with chlorhexidine solutions and applying an anti-infective ointment to the site of inflammation is importan [50-54].
The study included patients with diabetes mellitus who underwent prosthetics using dental implants. In order to confirm the importance of hygienic measures, the clinical indicators of implants and the effectiveness of implantation in the postoperative period were studied in patients who were under observation and received professional hygiene and as well in those patients who were left out of control and did not receive professional hygiene after implantation and consulted a doctor about various post-implantation problems. Compared to persons enrolled in the preventive protocol, those in the group without services were more likely to develop peri-implantitis (42.4% vs. 12,6%). The survival rate of implants after 3 years was 98.4%. The survival rate of implants after 3 years for those patients who were excluded from preventive services was 95.4%. To reduce the risk of implant failure and provide optimal conditions for rehabilitation and osseointegration, it is important to properly organize oral hygiene at home. This requires: carrying out thorough and as gentle cleaning as possible twice a day; using a soft or ultra-soft brush and toothpaste without whitening components or abrasives to care for your teeth; using a rinse recommended by the implantologist; treating the oral cavity with an antiseptic solution after each meal (treatment is carried out as a rinse); using an irrigator for high-quality cleansing of hard-to-reach places - it can be used a week after implantation of artificial roots. The main requirement when installing implants is stable compensation of the disease if the blood sugar level is less than 7 mmol/l..
In the subcompensated form, this figure is higher but does not exceed 14. Surgery in such a situation is extremely undesirable and is dangerous with complications. In the case of decompensated diabetes, elective surgery cannot be performed. Implantation is possible when the patient is in satisfactory condition. Diabetes mellitus is compensated, and the patient constantly receives maintenance therapy. An endocrinologist individually selects medications and confirms the stabilization of the process. There are no chronic disturbances in the functioning of the cardiovascular and circulatory systems: The patient does not smoke - nicotine constricts blood vessels, and insufficient blood flow greatly complicates healing; The diet is strictly observed - the diet is high in vitamins and low in carbohydrates, meals are frequent and in small portions; Dosed daily physical activity, stress effects are minimized; Oral hygiene is carried out extremely carefully; professional teeth cleaning has become a regular and familiar procedure. Implantation for diabetes mellitus is contraindicated in the following cases: developed complications - diabetic damage to the heart, kidneys, and liver; excess body weight; persistently high blood pressure; unstable course of the disease, the need to frequently adjust sugar levels; bleeding disorders. All these factors aggravate the course of the underlying disease and prevent any surgical procedures.
When planning dental implantation in patients with diabetes, it is fundamentally important to eliminate infectious diseases of the teeth and gums present in the oral cavity. After intervention, they can become a dangerous source of inflammation in bones and soft tissues, causing many complications. Problematic teeth should be treated in advance. In case of inflammation of the gums, periodontal treatment is performed. Professional oral hygiene is mandatory - it helps reduce the concentration of microorganisms on the teeth and mucous membranes. Potential inflammatory agents are removed along with soft and hard plaque. To monitor possible clinical changes, the patient should be examined every 6 months for the first year after implant restoration and problems identified by the presence of probing depth, bleeding on probing, suppuration, etc.
Carrying out the proposed preventive measures will increase the success of dental implantation in patients with diabetes. In general, these observations confirm the importance of individual prevention programs and constant monitoring. Study limited sample size (62) study focuses on a period, 2021 - 2023).
The lack of preventive measures in diabetic patients with functional dental implants has a negative impact on the long-term prognosis of the development of secondary inflammatory complications. patients with diabetes, regular medical examinations, accompanied by professional oral hygiene procedures, to prevent the development of negative reactions.
Declaration
Competing interest: The author declares that he has no competing interests. None of the authors have relevant financial relations with a commercial interest.
Ethical approval and consent to participate: The study was reviewed and approved by the University Ethical Committee and in accordance with those of the World Medical Association and the Helsinki Declaration.
Consent for publication: Patients were informed verbally and in writing about the study and gave written informed consent.
Availability of data and materials: All data generated or analysed during this study are included in this published article.
- Elani HW, Starr JR, Da Silva JD, Gallucci GO. Trends in Dental Implant Use in the U.S., 1999-2016, and Projections to 2026. J Dent Res. 2018 Dec;97(13):1424-1430. doi: 10.1177/0022034518792567. Epub 2018 Aug 3. PMID: 30075090; PMCID: PMC6854267.
- Buser D, Sennerby L, De Bruyn H. Modern implant dentistry based on osseointegration: 50 years of progress, current trends and open questions. Periodontol 2000. 2017 Feb;73(1):7-21. doi: 10.1111/prd.12185. PMID: 28000280.
- Sartoretto SC, Shibli JA, Javid K, Cotrim K, Canabarro A, Louro RS, Lowenstein A, Mourão CF, Moraschini V. Comparing the Long-Term Success Rates of Tooth Preservation and Dental Implants: A Critical Review. J Funct Biomater. 2023 Mar 3;14(3):142. doi: 10.3390/jfb14030142. PMID: 36976066; PMCID: PMC10055991.
- Papaspyridakos P, Chen CJ, Singh M, Weber HP, Gallucci GO. Success criteria in implant dentistry: a systematic review. J Dent Res. 2012 Mar;91(3):242-8. doi: 10.1177/0022034511431252. Epub 2011 Dec 8. PMID: 22157097.
- Moraschini V, Poubel LA, Ferreira VF, Barboza Edos S. Evaluation of survival and success rates of dental implants reported in longitudinal studies with a follow-up period of at least 10 years: a systematic review. Int J Oral Maxillofac Surg. 2015 Mar;44(3):377-88. doi: 10.1016/j.ijom.2014.10.023. Epub 2014 Nov 20. PMID: 25467739.
- Naujokat H, Kunzendorf B, Wiltfang J. Dental implants and diabetes mellitus-a systematic review. Int J Implant Dent. 2016 Dec;2(1):5. doi: 10.1186/s40729-016-0038-2. Epub 2016 Feb 11. PMID: 27747697; PMCID: PMC5005734.
- Chrcanovic BR, Albrektsson T, Wennerberg A. Diabetes and oral implant failure: a systematic review. J Dent Res. 2014 Sep;93(9):859-67. doi: 10.1177/0022034514538820. Epub 2014 Jun 13. PMID: 24928096; PMCID: PMC4541101.
- Wagner J, Spille JH, Wiltfang J, Naujokat H. Systematic review on diabetes mellitus and dental implants: an update. Int J Implant Dent. 2022 Jan 3;8(1):1. doi: 10.1186/s40729-021-00399-8. PMID: 34978649; PMCID: PMC8724342.
- Katyayan PA, Katyayan M, Shah RJ. Rehabilitative considerations for dental implants in the diabetic patient. J Indian Prosthodont Soc. 2013 Sep;13(3):175-83. doi: 10.1007/s13191-012-0207-9. Epub 2012 Nov 1. PMID: 24431731; PMCID: PMC3732704.
- Aronson D. Hyperglycemia and the pathobiology of diabetic complications. Adv Cardiol. 2008;45:1-16. doi: 10.1159/000115118. PMID: 18230953.
- Park JB. Bone healing at a failed implant site in a type II diabetic patient: clinical and histologic evaluations: a case report. J Oral Implantol. 2007;33(1):28-32. doi: 10.1563/0-826.1. PMID: 17410909.
- Berbudi A, Rahmadika N, Tjahjadi AI, Ruslami R. Type 2 Diabetes and its Impact on the Immune System. Curr Diabetes Rev. 2020;16(5):442-449. doi: 10.2174/1573399815666191024085838. PMID: 31657690; PMCID: PMC7475801.
- Lorenzo C, Okoloise M, Williams K, Stern MP, Haffner SM; San Antonio Heart Study. The metabolic syndrome as predictor of type 2 diabetes: the San Antonio heart study. Diabetes Care. 2003 Nov;26(11):3153-9. doi: 10.2337/diacare.26.11.3153. PMID: 14578254.
- Schalkwijk CG, Stehouwer CD. Vascular complications in diabetes mellitus: the role of endothelial dysfunction. Clin Sci (Lond). 2005 Aug;109(2):143-59. doi: 10.1042/CS20050025. PMID: 16033329.
- Spampinato SF, Caruso GI, De Pasquale R, Sortino MA, Merlo S. The Treatment of Impaired Wound Healing in Diabetes: Looking among Old Drugs. Pharmaceuticals (Basel). 2020 Apr 1;13(4):60. doi: 10.3390/ph13040060. PMID: 32244718; PMCID: PMC7243111.
- Dinh T, Elder S, Veves A. Delayed wound healing in diabetes: Considering future treatments. Diabetes Manag. 2011; 1:509–519. doi: 10.2217/dmt.11.44
- Greenhalgh DG. Wound healing and diabetes mellitus. Clin Plast Surg. 2003 Jan;30(1):37-45. doi: 10.1016/s0094-1298(02)00066-4. PMID: 12636214.
- Dasari N, Jiang A, Skochdopole A, Chung J, Reece EM, Vorstenbosch J, Winocour S. Updates in Diabetic Wound Healing, Inflammation, and Scarring. Semin Plast Surg. 2021 Aug;35(3):153-158. doi: 10.1055/s-0041-1731460. Epub 2021 Jul 15. PMID: 34526862; PMCID: PMC8432997.
- Nazir MA. Prevalence of periodontal disease, its association with systemic diseases and prevention. Int J Health Sci (Qassim). 2017 Apr-Jun;11(2):72-80. PMID: 28539867; PMCID: PMC5426403.
- Teeuw WJ, Gerdes VE, Loos BG. Effect of periodontal treatment on glycemic control of diabetic patients: a systematic review and meta-analysis. Diabetes Care. 2010 Feb;33(2):421-7. doi: 10.2337/dc09-1378. PMID: 20103557; PMCID: PMC2809296.
- Borgnakke WS, Ylöstalo PV, Taylor GW, Genco RJ. Effect of periodontal disease on diabetes: systematic review of epidemiologic observational evidence. J Periodontol. 2013 Apr;84(4 Suppl):S135-52. doi: 10.1902/jop.2013.1340013. PMID: 23631574.
- Latti BR, Kalburge JV, Birajdar SB, Latti RG. Evaluation of relationship between dental caries, diabetes mellitus and oral microbiota in diabetics. J Oral Maxillofac Pathol. 2018 May-Aug;22(2):282. doi: 10.4103/jomfp.JOMFP_163_16. PMID: 30158791; PMCID: PMC6097371.
- Hoseini A, Mirzapour A, Bijani A, Shirzad A. Salivary flow rate and xerostomia in patients with type I and II diabetes mellitus. Electron Physician. 2017 Sep 25;9(9):5244-5249. doi: 10.19082/5244. PMID: 29038704; PMCID: PMC5633220.
- Rohani B. Oral manifestations in patients with diabetes mellitus. World J Diabetes. 2019 Sep 15;10(9):485-489. doi: 10.4239/wjd.v10.i9.485. PMID: 31558983; PMCID: PMC6748880.
- Al-Maskari AY, Al-Maskari MY, Al-Sudairy S. Oral Manifestations and Complications of Diabetes Mellitus: A review. Sultan Qaboos Univ Med J. 2011 May;11(2):179-86. Epub 2011 May 15. PMID: 21969888; PMCID: PMC3121021.
- Indurkar MS, Maurya AS, Indurkar S. Oral Manifestations of Diabetes. Clin Diabetes. 2016 Jan;34(1):54-7. doi: 10.2337/diaclin.34.1.54. PMID: 26807010; PMCID: PMC4714722.
- Cicmil A, Govedarica O, Lečić J, Mališ S, Cicmil S, Čakić S. Oral Symptoms and Mucosal Lesions in Patients with Diabetes Mellitus Type 2. Balk J Dent Med. 2017; 21:50–54.
- Mauri-Obradors E, Estrugo-Devesa A, Jané-Salas E, Viñas M, López-López J. Oral manifestations of Diabetes Mellitus. A systematic review. Med Oral Patol Oral Cir Bucal. 2017 Sep 1;22(5):e586-e594. doi: 10.4317/medoral.21655. PMID: 28809366; PMCID: PMC5694181.
- Yang S, Li Y, Liu C, Wu Y, Wan Z, Shen D. Pathogenesis and treatment of wound healing in patients with diabetes after tooth extraction. Front Endocrinol (Lausanne). 2022 Sep 23; 13:949535. doi: 10.3389/fendo.2022.949535. PMID: 36213270; PMCID: PMC9538860.
- Yamano S, Kuo WP, Sukotjo C. Downregulated gene expression of TGF-βs in diabetic oral wound healing. J Craniomaxillofac Surg. 2013 Mar;41(2):e42-8. doi: 10.1016/j.jcms.2012.08.001. Epub 2012 Sep 7. PMID: 22964221.
- Radović K, Brković B, Roganović J, Ilić J, Milić Lemić A, Jovanović B. Salivary VEGF and post-extraction wound healing in type 2 diabetic immediate denture wearers. Acta Odontol Scand. 2022 Jan;80(1):9-14. doi: 10.1080/00016357.2021.1930149. Epub 2021 May 25. PMID: 34033524.
- de Morais JA, Trindade-Suedam IK, Pepato MT, Marcantonio E Jr, Wenzel A, Scaf G. Effect of diabetes mellitus and insulin therapy on bone density around osseointegrated dental implants: a digital subtraction radiography study in rats. Clin Oral Implants Res. 2009 Aug;20(8):796-801. doi: 10.1111/j.1600-0501.2009.01716.x. Epub 2009 May 26. PMID: 19486078.
- Dowell S, Oates TW, Robinson M. Implant success in people with type 2 diabetes mellitus with varying glycemic control: a pilot study. J Am Dent Assoc. 2007 Mar;138(3):355-61; quiz 397-8. doi: 10.14219/jada.archive.2007.0168. PMID: 17332041.
- Dubey RK, Gupta DK, Singh AK. Dental implant survival in diabetic patients; review and recommendations. Natl J Maxillofac Surg. 2013 Jul;4(2):142-50. doi: 10.4103/0975-5950.127642. PMID: 24665167; PMCID: PMC3961886.
- Khandelwal N, Oates TW, Vargas A, Alexander PP, Schoolfield JD, Alex McMahan C. Conventional SLA and chemically modified SLA implants in patients with poorly controlled type 2 diabetes mellitus--a randomized controlled trial. Clin Oral Implants Res. 2013 Jan;24(1):13-9. doi: 10.1111/j.1600-0501.2011.02369.x. Epub 2011 Dec 6. PMID: 22145978.
- Picke AK, Campbell G, Napoli N, Hofbauer LC, Rauner M. Update on the impact of type 2 diabetes mellitus on bone metabolism and material properties. Endocr Connect. 2019 Mar 1;8(3):R55-R70. doi: 10.1530/EC-18-0456. PMID: 30772871; PMCID: PMC6391903.
- Murray CE, Coleman CM. Impact of Diabetes Mellitus on Bone Health. Int J Mol Sci. 2019 Sep 30;20(19):4873. doi: 10.3390/ijms20194873. PMID: 31575077; PMCID: PMC6801685.
- Kochar SP, Reche A, Paul P. The Etiology and Management of Dental Implant Failure: A Review. Cureus. 2022 Oct 19;14(10):e30455. doi: 10.7759/cureus.30455. PMID: 36415394; PMCID: PMC9674049.
- Rokaya D, Srimaneepong V, Wisitrasameewon W, Humagain M, Thunyakitpisal P. Peri-implantitis Update: Risk Indicators, Diagnosis, and Treatment. Eur J Dent. 2020 Oct;14(4):672-682. doi: 10.1055/s-0040-1715779. Epub 2020 Sep 3. PMID: 32882741; PMCID: PMC7536094.
- Renvert S, Persson GR, Pirih FQ, Camargo PM. Peri-implant health, peri-implant mucositis, and peri-implantitis: Case definitions and diagnostic considerations. J Clin Periodontol. 2018 Jun;45 Suppl 20:S278-S285. doi: 10.1111/jcpe.12956. PMID: 29926496.
- Gulati M, Govila V, Anand V, Anand B. Implant Maintenance: A Clinical Update. Int Sch Res Notices. 2014 Jul 9;2014:908534. doi: 10.1155/2014/908534. PMID: 27437506; PMCID: PMC4897104.
- Silverstein LH, Kurtzman GM. Oral hygiene and maintenance of dental implants. Dent Today. 2006 Mar;25(3):70-5; quiz 75. PMID: 16617795.
- Garg AK, Duarte F, Funari K. Hygeinic maintenance of dental implants. Journal of Practical Hygiene. 1997; 6(2):13–17.
- Dukka H, Saleh MHA, Ravidà A, Greenwell H, Wang HL. Is bleeding on probing a reliable clinical indicator of peri-implant diseases? J Periodontol. 2021 Dec;92(12):1669-1674. doi: 10.1002/JPER.20-0890. Epub 2021 May 10. PMID: 33829501.
- Monje A, Insua A, Rakic M, Nart J, Moyano-Cuevas JL, Wang HL. Estimation of the diagnostic accuracy of clinical parameters for monitoring peri-implantitis progression: An experimental canine study. J Periodontol. 2018 Dec;89(12):1442-1451. doi: 10.1002/JPER.18-0081. Epub 2018 Aug 16. PMID: 30014465.
- Polymeri A, Loos BG, Aronovich S, Steigmann L, Inglehart MR. Risk factors, diagnosis, and treatment of peri-implantitis: A cross-cultural comparison of U.S. and European periodontists' considerations. J Periodontol. 2022 Apr;93(4):481-492. doi: 10.1002/JPER.21-0010. Epub 2021 Oct 19. PMID: 34390497; PMCID: PMC10138758.
- Scarano A, Khater AGA, Gehrke SA, Serra P, Francesco I, Di Carmine M, Tari SR, Leo L, Lorusso F. Current Status of Peri-Implant Diseases: A Clinical Review for Evidence-Based Decision Making. J Funct Biomater. 2023 Apr 10;14(4):210. doi: 10.3390/jfb14040210. PMID: 37103300; PMCID: PMC10142594.
- Renvert S, Hirooka H, Polyzois I, Kelekis-Cholakis A, Wang HL; Working Group 3. Diagnosis and non-surgical treatment of peri-implant diseases and maintenance care of patients with dental implants - Consensus report of working group 3. Int Dent J. 2019 Sep;69(Suppl 2):12-17. doi: 10.1111/idj.12490. PMID: 31478575; PMCID: PMC9379037.
- Stiesch M, Grischke J, Schaefer P, Heitz-Mayfield LJA. Supportive care for the prevention of disease recurrence/progression following peri-implantitis treatment: A systematic review. J Clin Periodontol. 2023 Jun;50 Suppl 26:113-134. doi: 10.1111/jcpe.13822. Epub 2023 Jun 20. PMID: 37339881.
- Wada M, Mameno T, Otsuki M, Kani M, Tsujioka Y, Ikebe K. Prevalence and risk indicators for peri-implant diseases: A literature review. Jpn Dent Sci Rev. 2021 Nov; 57:78-84. doi: 10.1016/j.jdsr.2021.05.002. Epub 2021 Jun 8. PMID: 34158874; PMCID: PMC8203834.
- Hultin M, Komiyama A, Klinge B. Supportive therapy and the longevity of dental implants: a systematic review of the literature. Clin Oral Implants Res. 2007 Jun;18 Suppl 3:50-62. doi: 10.1111/j.1600-0501.2007.01447.x. Erratum in: Clin Oral Implants Res. 2008 Mar;19(3):326-8. PMID: 17594370.
- Dental Implants Facts and Figures. American Academy of Implant Dentistry website. https://www.aaid.com/about/Press_Room/Dental_Implants_FAQ.html. Accessed March 20, 2017
- Dumitriu AS, Păunică S, Nicolae XA, Bodnar DC, Albu ȘD, Suciu I, Ciongaru DN, Giurgiu MC. The Effectiveness of the Association of Chlorhexidine with Mechanical Treatment of Peri-Implant Mucositis. Healthcare (Basel). 2023 Jul 3;11(13):1918. doi: 10.3390/healthcare11131918. PMID: 37444752; PMCID: PMC10341060.
- Tarawali K. Maintenance and Monitoring of Dental Implants in General Dental Practice. Dent Update. 2015 Jul-Aug;42(6):513-4, 517-8. doi: 10.12968/denu.2015.42.6.513. PMID: 26506806.